According to Mayo Clinic research, Single leg balance is the most sensitive indicator of neuromuscular ageing. This finding provides valuable insights about strength and gait measurements in health assessment.
The scientific data behind single leg balance highlights its benefits in health evaluation. Studies demonstrate this measure outperforms standard indicators in predicting age-related decline. Understanding this relationship requires examining the relationship between multiple body systems.
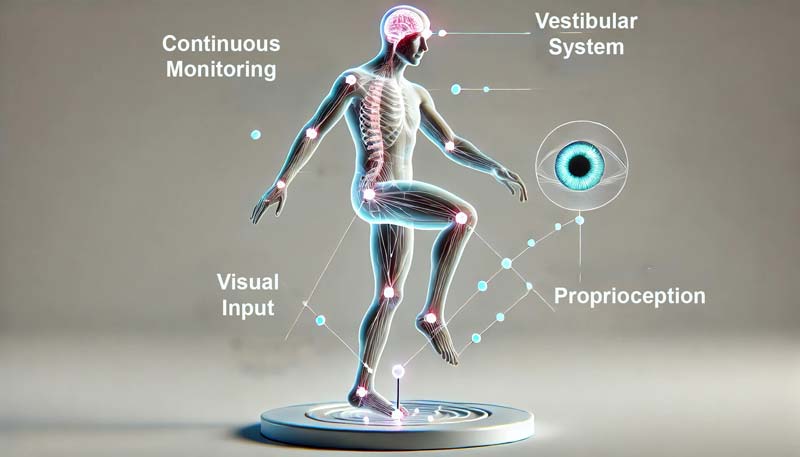
Picture a precision timepiece where every component must work in perfect harmony. The vestibular system (balance mechanisms in your inner ear) coordinates with visual input and proprioception (your body’s position awareness). These systems work together, creating a real-time feedback loop for stability.
Age brings notable changes to this delicate balance system. Research shows older adults activate different muscle patterns than younger individuals when maintaining stability. These adaptations reveal how our bodies compensate for age-related changes.
The duration someone can maintain single leg balance offers crucial insights into overall health status. Studies demonstrate that this test correlates strongly with mortality risk and functional independence. This relationship stems from balance’s unique role in coordinating multiple physiological systems.
Evidence points to balance assessment as a powerful window into neuromuscular health. Understanding these mechanisms helps explain why single-leg balance is a reliable indicator of age-related changes. The following sections explore this relationship in detail.
Why Single Leg Balance Matters for Your Health
Research identifies falls as the primary cause of injuries among adults aged 65 and older. The ability to maintain a single leg balance provides crucial insights into fall risk assessment.
The Mayo Clinic study reveals striking data about balance capabilities. Measurements of single leg balance outperform traditional tests in predicting age-related decline. This finding transforms our understanding of health assessment. Statistics paint a clear picture of balance’s importance:
- Individuals unable to hold their balance for 10 seconds show 84% higher mortality risk
- Balance decline starts at 2.2 seconds per decade on the non-dominant leg
- Loss of balance causes most falls in older populations
- Early balance changes can signal developing health issues
Balance testing reveals crucial information about neurological function. Studies show strong correlations between balance ability and peripheral neuropathy (nerve damage in extremities). This connection helps identify potential nerve problems before symptoms become severe.
Healthcare professionals now recognize balance as a vital health indicator. Testing protocols examine:
- Duration of stable stance
- Quality of balance maintenance
- Compensation patterns
- Side-to-side differences
The implications reach across multiple health domains. Poor balance correlates with:
- Increased risk of falls
- Reduced physical activity
- Lower functional independence
- Greater healthcare needs
This knowledge about balance capabilities helps individuals and healthcare providers create or develop targeted interventions. Early identification of balance issues allows for proactive treatment approaches. This can significantly impact long-term health outcomes.
The Science Behind Balance Testing
Balance maintenance works like a high-performance vehicle’s stability system. The body coordinates multiple systems to maintain single leg balance through continuous adjustments.
Data from balance testing reveals fascinating insights about muscle activation. Older adults show distinct patterns during single leg balance compared to younger individuals. These differences highlight age-related adaptations.
The body employs three primary systems for balance control:
1: Vestibular System (Inner Ear)
- Monitors head position and movement
- Provides information about spatial orientation
- Helps maintain visual stability during motion
2: Visual Input
- Processes environmental information
- Assists with spatial awareness
- Helps anticipate balance challenges
3: Proprioception (Position Sense)
- Tracks body position in space
- Monitors muscle and joint movements
- Provides feedback about stability
Research demonstrates how these systems work together. The process involves:
- Continuous monitoring of body position
- Rapid processing of sensory information
- Immediate muscle response adjustments
- Real-time balance corrections
Age brings significant changes to this system. Studies show:
- Increased reliance on visual input
- Modified muscle activation patterns
- Altered response times
- Different balance strategies
Brain involvement plays a crucial role in balance maintenance. The process requires:
- Active sensory integration
- Motor planning and execution
- Rapid response capabilities
- Adaptive strategy selection
These mechanisms help explain why balance testing proves so valuable. The assessment examines:
- System integration effectiveness
- Compensation capabilities
- Neural processing speed
- Overall balance strategy
Age-Related Balance Standards: What You Should Achieve
Scientific research establishes clear standards for single leg balance across age groups. The Mayo Clinic study reveals significant patterns in balance capabilities, with steady declines occurring throughout life.
Through extensive testing, researchers identified optimal balance times for each age bracket. The data demonstrates how single leg balance capabilities naturally shift with age. A fascinating aspect emerges when examining these standards – they tell a story of our body’s adaptation through time.
Ages 18-39: 43 seconds
Your balance abilities peak during these years. Think of it as your physiological prime – much like professional athletes who typically achieve their best performances in this window.
Ages 40-49: 40 seconds
A subtle decline begins, though most people barely notice. The body maintains remarkable balance capabilities, requiring only minor adjustments to maintain stability.
Ages 50-59: 37 seconds
Balance adaptations become more pronounced. The body employs additional compensatory mechanisms to maintain stability, particularly in the hip and ankle regions.
Ages 60-69: 30 seconds
This decade marks a significant transition point. The Mayo Clinic research identified this period as crucial for implementing preventative balance training.
Ages 70-79: 18 seconds
Balance strategies shift significantly. The body relies more heavily on visual input and altered muscle activation patterns to maintain stability.
Ages 80+: 5 seconds
While shorter, this duration still indicates functional independence. Many individuals maintain active lifestyles despite reduced balance times.
These standards apply specifically to eyes-open conditions. For advanced assessment, and for those who are daring, you can test your balance with eyes closed, and these are the target times:
- Ages 18-39: 9 seconds
- Ages 40-49: 7 seconds
- Ages 50-59: 5 seconds
- Ages 60-69: 3 seconds
- Ages 70-79: 2 seconds
- Ages 80+: 1 second
The research identifies critical factors affecting balance performance. These include:
Environmental Conditions
- Lighting levels
- Surface stability
- Temperature control
- Surrounding distractions
Physical Factors
- Overall fitness level
- Previous injuries
- Medication effects
- Time of day
Neurological Elements
- Visual processing
- Vestibular function
- Proprioceptive feedback
- Neural response time
Simple Ways to Test and Improve Your Single Leg Balance
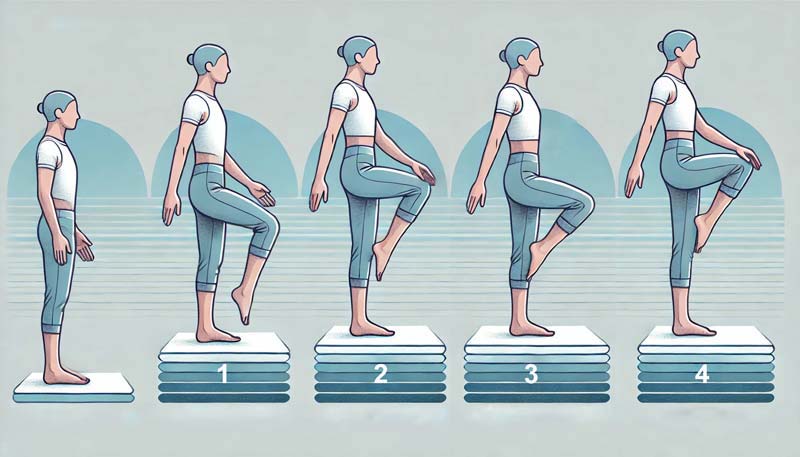
Scientific evidence supports specific protocols for enhancing single leg balance abilities. Research demonstrates notable improvements through structured training approaches.
The Mayo Clinic findings highlight the importance of targeted exercise progression. Improving single leg balance requires a systematic approach, combining various training elements.
Balance Training Fundamentals
Start with a thorough assessment of current capabilities. Scientific protocols recommend specific progression pathways through static and dynamic exercises.
Static Exercise Progression
- Bipedal stance (feet together)
- Semi-tandem stance (feet partially aligned)
- Tandem stance (heel-to-toe position)
- Single leg stance
Dynamic Training Elements
- Multi-directional movements
- Speed variations
- Rhythmic adjustments
- Directional changes
Research validates specific training parameters for optimal results. Each session should maintain:
Time Parameters
- Total duration: 45 minutes
- Individual exercises: 30 seconds
- Rest intervals: 2 minutes
- Frequency: 3 sessions weekly
Training Variables
- Surface variations (firm to unstable)
- Visual conditions (eyes open/closed)
- Movement directions (forward/backward/lateral)
- Speed adjustments (slow to fast)
Advanced balance training incorporates additional elements. Scientific studies support including reactive balance work:
- Controlled perturbations
- Multi-directional challenges
- Speed variations
- Amplitude adjustments
The evidence supports specific intensity guidelines. Exercise sessions should target intensity levels:
- Beginners: RPE 12-13 (somewhat hard)
- Intermediate: RPE 13-14 (moderately hard)
- Advanced: RPE 14-16 (hard)
Safety considerations remain paramount throughout training. Research establishes precise prerequisites. Essential safety measures should consist of the following:
- Proper environment setup
- Adequate lighting
- Support structures nearby
- Professional supervision when needed
Success indicators help track progress effectively. Progress markers to consider are:
- Increased stance duration
- Reduced sway measurements
- Improved dual-task performance
- Enhanced gait stability
The Mayo Clinic research transforms a simple one-legged stance into a powerful health assessment tool. This elegant test requires no special equipment yet reveals deep insights about neuromuscular ageing, overall health, and longevity.
Balance testing serves as a notable window into our body’s elaborate systems. From revealing age-related changes to identifying early warning signs, this straightforward measurement speaks volumes about our health journey through time.
Sources
- Amiridis IG, Hatzitaki V, Arabatzi F. Age-induced modifications of static postural control in humans. Neurosci Lett. 2003;350(3):137–40.
- Ferrucci L, Cooper R, Shardell M, Simonsick EM, Schrack JA, Kuh D. Age-related change in mobility: perspectives from life course epidemiology and geroscience. Journals of gerontology series a: biomedical sciences and medical sciences. 2016;71(9):1184–94.
- Granacher U, et al. Effects of a salsa dance training on balance and strength performance in older adults. Gerontology. 2011;58:305–312.
- Granacher U, Muehlbauer T, Zahner L, Gollhofer A, Kressig RW. Comparison of traditional and recent approaches in the promotion of balance and strength in older adults. Sports Med. 2011;41(5):377–400.)
- Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age and ageing. 2006;35(suppl_2):ii7–ii11.
- Hurvitz EA, Richardson JK, Werner RA. Unipedal stance testing in the assessment of peripheral neuropathy. Archives of physical medicine and rehabilitation. 2001;82(2):198–204.
- Le Mouel C, Brette R. Anticipatory coadaptation of ankle stiffness and sensorimotor gain for standing balance. PLoS Comput Biol. 2019;15(11):e1007463.
- Lubetzky AV, Soroka A, Harel D, et al. Static and dynamic balance in adults undergoing lumbar spine surgery: screening and prediction of postsurgical outcomes. J Am Acad Orthop Surg. 2020;28:e553–9.
- MacKinnon CD. Sensorimotor anatomy of gait, balance, and falls. Handb Clin Neurol. 2018;159:3–26.
- Neumann DA. Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther. 2010;40(2):82–94.
- Pescatello LS, et al. Sneak Peek: preview of ACSM’s guidelines for exercise testing and prescription. ACSMs Health Fit J. 2013;17:16-20.
- Rezaei A, Bhat SG, Cheng CH, Pignolo RJ, Lu L, Kaufman KR. Age-related changes in gait, balance, and strength parameters: A cross-sectional study. PLoS One. 2024 Oct 23;19(10):e0310764.
- Sherrington C, et al. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med 2020;54:885–91.
- Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther. 2007;30(1):8-15.
- Sturnieks DL, et al. Sensorimotor and neuropsychological correlates of force perturbations that induce stepping in older adults. Gait Posture. 2012;36(3):356–360.
- Tanaka EH, Santos PF, Reis JG, Rodrigues NC, Moraes R, Abreu DC. Is there a relationship between complaints of impaired balance and postural control disorder in community-dwelling elderly women? Braz J Phys Ther. 2015;19(3):186–93.
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One‐leg balance is an important predictor of injurious falls in older persons. Journal of the American Geriatrics Society. 1997;45(6):735–8.