The impact of cancer on physical health is profoundly marked in cancer treatments like chemotherapy, radiation, and surgery. Cancer, comprising over 200 distinct diseases, is characterised by uncontrolled cell growth.
This is often due to genetic mutations affecting various tissues such as epithelial (carcinoma), connective (sarcomas), bone (blastoma), blood (leukaemia), or lymph nodes (lymphoma). The progression of cancer is staged from 0, denoting localised abnormal cells, to 4, indicating metastasis.
Cancer treatments, while targeting malignant cells, also often damage healthy tissue, leading to limitations in physical abilities during and post-treatment. These side effects can significantly diminish overall bodily function. Even years after treatment, many survivors continue to report physical limitations, underscoring the long-term impact of cancer treatments on physical health.
This post aims to unpack how cancer treatments impact physical health, examining patients’ various challenges. We will explore the effects of treatments on physical well-being and discuss strategies for managing and mitigating these impacts.
I will present detailed insights into tailored exercise and rehabilitation approaches to aid recovery, manage symptoms, and enhance physical fitness for cancer survivors.
Impact of Cancer on Physical Health: Effects on Strength and Endurance
The Impact of Cancer on Physical Health, particularly concerning strength and endurance, is significant. Cancer treatments such as surgery, radiation, chemotherapy, hormones, and immunotherapy, while crucial in combating cancer cells, often cause collateral damage to healthy tissues. This leads to adverse effects that restrict exercise capability during and post-treatment, profoundly affecting physical health.
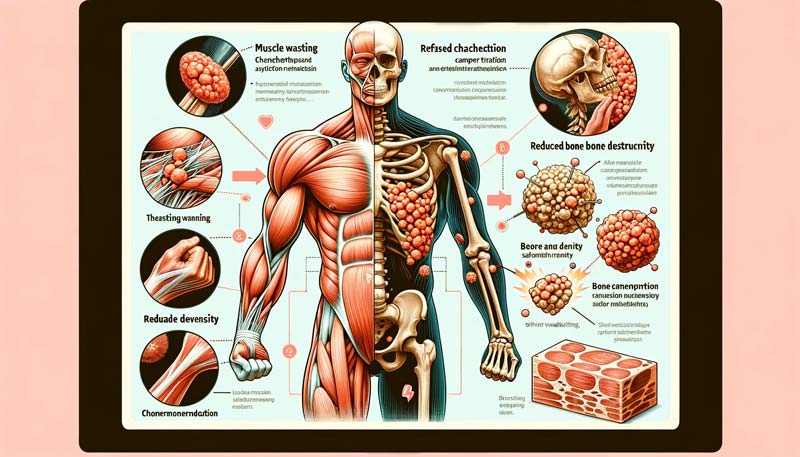
Cachexia, or muscle wasting, notably affects individuals with advanced gastrointestinal cancers, limiting exercise capacity and thus further illustrating the impact of cancer on physical health.
Bone metastases compel patients to modify their exercise routines, considering the increased risk of fractures. The heightened infection risk during chemotherapy or radiation underscores the need for careful exercise planning.
Up to 90% of cancer survivors experience cancer-related fatigue, a critical aspect of the impact of cancer on the physical body. This fatigue is particularly prevalent during chemotherapy and radiation and can persist long after treatment, affecting the ability to exercise.
Peripheral neuropathies, resulting from nerve damage during surgery, manifest as muscle weakness and balance issues, contributing to the overall impact of cancer on physical health. Hormone therapy, vital in cancer treatment, can lead to reduced bone mass and density.
More than half of the cancer survivors, even years after treatment, report limitations in physical activities. The progression in exercise frequency and intensity for these individuals might be slower than that for healthy adults, with maintaining physical function or fitness often becoming a primary exercise goal.

Limitations on Physical Function Due to Treatment
Treatments, targeting cancer cells, often inadvertently harm healthy tissues. This leads to side effects that limit exercise ability during and post-treatment, highlighting the significant
impact of cancer on physical health.Overall, physical function is generally reduced in cancer survivors. Post-treatment, many individuals experience limitations in basic physical activities, a testament to the enduring impact of cancer.
This includes difficulty crouching, kneeling, standing for extended periods, and carrying moderate weights. Even simple activities like walking short distances can become challenging.
Ionising radiation, a standard treatment modality, continues to affect the treated body areas for life. The radiation scatter can damage healthy tissue, with effects localised to the irradiated body part. For example, chest wall radiation may cause heart arrhythmias and pulmonary fibrosis, while radiation lower on the torso can lead to gastrointestinal changes like irritable bowel syndrome.
Nerve damage during surgery, can also present as numbness, or ataxia. This can lead to muscle weakness and balance issues, restricting the range of motion around affected joints. Hormone therapy, crucial for reducing tumour-growth-promoting hormones, can also adversely affect bone health, increasing fracture risks.
The systemic effects of chemotherapy are varied, depending on the drug class. For instance, anthracyclines used in breast cancer treatment can damage the heart, increasing the risk of cardiomyopathies and heart failure. In contrast, platinum-based chemotherapy drugs commonly cause peripheral neuropathy, potentially leading to long-term sensory and motor function impairment.
Cancer-related fatigue, prevalent in patients undergoing chemotherapy and radiation, can significantly restrict exercise ability. This fatigue, part of the broader impact of cancer on physical health, may persist for months or years post-treatment. However, avoiding physical inactivity and engaging in aerobic exercise are advised, given the positive effects on fatigue management.
Adapting Exercise for Changing Abilities
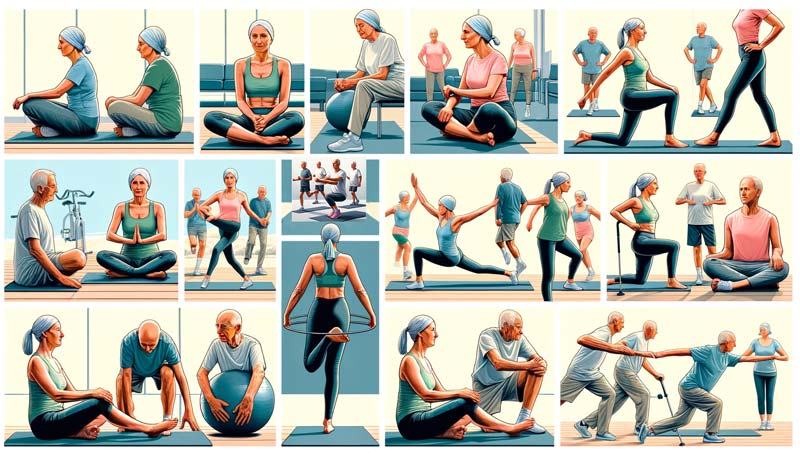
Adapting exercise programs for cancer survivors is a crucial and nuanced journey towards reclaiming strength and endurance, particularly in light of the impact of cancer on physical health. The profound impact of cancer on physical health often necessitates a tailored approach to exercise, one that respects the body’s altered state post-treatment.
These programs need to be dynamic, evolving with the recuperating capabilities of survivors. This bespoke approach is pivotal in fostering both physical and psychological recovery. For many, maintaining physical function becomes a primary goal, necessitating careful monitoring for symptoms like fatigue, muscle weakness, or swelling.
Transitioning to a personalised exercise routine involves several critical adjustments. These adaptations are transformative steps in a survivor’s path to wellness.
Below, we will explore these adaptations, each underpinned by rigorous scientific research, ensuring that every movement and milestone aligns with the unique needs of cancer patients.
- Gradual Increase in Exercise Intensity: Cancer survivors may need to progress in exercise frequency, intensity, and duration more slowly than healthy individuals. This is to avoid exacerbating symptoms like fatigue and muscle weakness.
- Safety Measures for Balance and Bone Health: Special attention is required for those with balance issues or reduced bone mineral density. Low-impact aerobic exercises, controlled resistance movements, and seated flexibility exercises can enhance safety and minimise fall risks.
- Customised Exercises for Neuropathy and Hormone Therapy Effects: Tailoring exercises to manage peripheral neuropathy symptoms and considering the effects of hormone therapy on bone health are essential. This includes low-intensity, weight-bearing exercises and pain management strategies.
- Low-Resistance Training and Lymphedema Management: Starting resistance training at a very low intensity and gradually increasing it is crucial, especially for breast cancer survivors with lymphedema. Monitoring for changes in swelling and using appropriate pressure garments during exercise is recommended.
- Exercise Variability for Treatment Tolerance: Exercise tolerance can fluctuate, particularly during active treatment phases. Adapting exercise intensity and duration according to the treatment schedule and individual response is vital.
- Individualisation of Exercise Programs: The overall exercise prescription should be highly individualised, considering the type of cancer, treatment phase, side effects, and physical impairments. This approach ensures that the exercise program evolves with the survivor’s recovery journey.
- Incorporating Flexibility and Balance Exercises: Including flexibility training to maintain range of motion. And balance exercises for fall prevention are essential, especially for those experiencing neuropathy, weakness, or unsteady gait.
- Adaptations for Cardiovascular Deconditioning: Monitoring for cardiovascular deconditioning and adjusting exercise intensity or duration is critical. This may include incorporating resistive exercises into a walking program.
- Gentle Movement-Based Exercises: For those limited by fatigue, neuropathy, or bone loss, gentle exercises such as yoga, Tai Chi, or Qigong can offer beneficial alternatives.
- Aquatic Exercises for Joint Support: Water-based exercises can provide joint stabilisation and compression, reducing muscle and common strain, which is especially beneficial for very weak or obese patients.
- Seated Exercise Options: For those unable to engage in weight-bearing activities, seated exercises like arm raises, cycling, and marching can help maintain baseline fitness levels.
- Supervised Exercise for Optimised Adaptations: Supervised exercise allows for modification of program variables based on acute patient response, optimising long-term adaptations.

Special Considerations for Bone Health Amid the Impact of Cancer on Physical Health
Cancer treatments profoundly influence bone health, raising challenges that go beyond immediate therapeutic effects. The onset of osteoporosis and increased fracture risks, particularly in patients undergoing hormone therapy and chemotherapy, mark a significant impact of cancer on physical health.
Bone density concerns are side effects and life-altering conditions that demand meticulous management and adaptation.
Patients receiving treatments like androgen deprivation therapy or aromatase inhibitors face accelerated bone loss, transforming the landscape of their physical health. This bone fragility necessitates a delicate balance in exercise and daily activities to fortify bone strength while mitigating fracture risks.
Addressing these concerns requires a comprehensive understanding of the complex interplay between cancer treatments and bone metabolism. Adapting to these challenges involves several critical considerations, each supported by thorough research and clinical insights. Let’s look into these vital adaptations:
- Monitoring and Modifying Exercise for Bone Metastases: Patients with bone metastases must carefully adjust their exercise programs, balancing physical activity and the risk of skeletal fractures. This calls for a nuanced approach to exercise intensity and mode.
- Managing Hormone Therapy Effects on Bone Density: Treatments like androgen deprivation therapy and aromatase inhibitors, crucial in cancer management, unfortunately contribute to rapid bone loss. Exercise programmes need to account for this, focusing on activities that strengthen bones without imposing excessive strain.
- Tailored Exercises for Increased Fracture Risks: The heightened fracture risks associated with specific cancer treatments demand a specialised exercise approach. This includes incorporating low-impact, bone-strengthening activities and avoiding high-risk movements.
- Protective Strategies for Osteoporosis: Cancer survivors facing osteoporosis require exercise modifications to prevent fractures. This involves integrating balance training, supported exercises, and avoiding high-impact activities.
- Supervised Exercise for Safe Bone Strengthening: For those with significant bone loss, managed exercise programs can offer safe and effective means to enhance bone health, using appropriate modifications like reduced loads and carefully monitored resistance training.
- Navigating Bone Health Post-Chemotherapy: The bone loss associated with chemotherapy, especially in premenopausal women, calls for careful monitoring and tailored exercise plans to mitigate rapid bone density reduction.
- Bone Density Preservation in Hormone-Receptor Positive Breast Cancer: Patients on aromatase inhibitors for breast cancer face unique challenges in maintaining bone health. Exercise programs for these individuals must be specifically adapted to counteract the accelerated bone loss characteristic of their treatment.
- Mitigating Bone Loss from Androgen Deprivation Therapy: Prostate cancer patients undergoing androgen deprivation therapy experience significant bone density reduction, increasing their fracture risks. Exercise programs for these patients should be crafted to strengthen bones while acknowledging their heightened vulnerability.
- Exercise Modifications for Bone Metastasis-Related Pain: Addressing the pain and reduced mobility from bone metastases is vital. Tailored exercise plans can help maintain physical function and mitigate pain, enhancing overall well-being.
- Bone Health in the Context of Overall Cancer Rehabilitation: The overarching goal in addressing bone health amid cancer treatment is to integrate these considerations into a holistic cancer rehabilitation program. This approach ensures that bone health is not viewed in isolation but as a crucial component of comprehensive survivorship care.
As we close this exploration of the impact of cancer on physical health, it’s clear that the path through and beyond cancer is both complex and deeply personal. It’s a route marked by resilience, adaptation, and continuous learning.
For every survivor, caregiver, and healthcare professional, understanding these nuances of cancer’s impact – especially on bone health – it’s about medical management and empowering each individual to steer this journey with strength, knowledge, and hope.
The insights shared here aim to light the way forward, illuminating the path towards recovery, well-being, and a renewed sense of vitality in the face of cancer’s challenges.
Sources
- Amir E, Seruga B, Niraula S, Carlsson L, Ocaña A. “Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis.” Journal of the National Cancer Institute, 2011;103(17):1299-1309.
- Brown JC, Huedo-Medina TB, Pescatello LS, Pescatello SM, Ferrer RA, Johnson BT. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: a metaanalysis. Cancer Epidemiol Biomarkers Prev. 2011;20(1):123–33.
- Cormie, Prue, Zopf, Eva M., Zhang, Xiaochen, et al. “The Impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects.” Epidemiologic Reviews, 2017;39(1):71-92.
- Courneya, Kerry S., Segal, Roanne J., Mackey, John R., et al. “Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial.” Journal of Clinical Oncology, 2007;25(28):4396-4404.
- Galantino, Mary Lou, Green, Lisa, DeCesari, Jennifer A., et al. “Safety and feasibility of modified chair‐yoga on functional outcome among elderly at risk for falls.” International Journal of Yoga, 2012;5(2):146.
- Galvão DA, Taaffe DR, Spry N, Joseph D, Newton RU. “Combined resistance and aerobic exercise program reverses bone loss in men treated with androgen suppression therapy for prostate cancer without bone metastases: a randomized controlled trial.” Journal of Clinical Oncology, 2010;28(2):340–7.
- Hadji P, Aapro MS, Body JJ, et al. “Management of aromatase inhibitor-associated bone loss in postmenopausal women with breast cancer: practical guidance for prevention and treatment.” Annals of Oncology, 2011;22(12):2546-2555.
- Handforth C, D’Oronzo S, Coleman R, Brown J. “Cancer Treatment and Bone Health.” Calcified Tissue International, 2018;102(2):251-264.
- Hewitt, M. Elizabeth., Greenfield, Sheldon., & Stovall, Ellen. (2006). From cancer patient to cancer survivor : lost in transition. National Academies Press.
- Jones LW, Courneya KS, Mackey JR, et al. Cardiopulmonary function and age-related decline across the breast cancer survivorship continuum. J Clin Oncol. 2012;30:2530–7.
- Kilbreath, Sharon L., Refshauge, Kathryn M., Beith, Janice M., et al. “Upper limb progressive resistance training and stretching exercises following surgery for early breast cancer: a randomized controlled trial.” Breast Cancer Research and Treatment, May 2012;133(2):667-76.
- Kong P, Yan J, Liu D, et al. “Skeletal-related events and overall survival of patients with bone metastasis from non-small cell lung cancer—A retrospective analysis.” Medicine (Baltimore), 2017;96(51):e9327.
- Ness KK, Wall MM, Oakes JM, Robison LL, Gurney JG. Physical performance limitations and participation restrictions among cancer survivors: a population-based study. Ann Epidemiol. 2006;16(3):197–205.
- Nilsen TS, Raastad T, Skovlund E, Courneya KS, Langberg CW, Lilleby W, Fosså SD, Thorsen L. Effects of strength training on body composition, physical functioning, and quality of life in prostate cancer patients during androgen deprivation therapy. Acta Oncol. 2015 Nov;54(10):1805-13.
- Petrick JL, Reeve BB, Kucharska-Newton AM, et al. Functional status declines among cancer survivors: trajectory and contributing factors. J Geriatr Oncol. 2014;5(4):359–67.
- Schmitz KH, Ahmed RL, Troxel AB, et al. Weight lifting for women at risk for breast cancerrelated lymphedema: a randomized trial. JAMA. 2010;304(24):2699-2705.
- Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvão DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL; American College of Sports Medicine. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010 Jul;42(7):1409-26.
- Schneider, Carole M., Hsieh, Ching C., Sprod, Lisa K., Carter, Scott D., Hayward, Reid. “Effects of supervised exercise training on cardiopulmonary function and fatigue in breast cancer survivors during and after treatment.” Cancer, 2007;110(4):918-925.
- Schwartz AL, Winters-Stone K. “Effects of a 12-month randomized controlled trial of aerobic or resistance exercise during and following cancer treatment in women.” Physician and Sportsmedicine, 2009;37(3):62-67.
- Schneider CM, Dennehy CA, Roozeboom M, Carter SD. A model program: exercise intervention for cancer rehabilitation. Integr Cancer Ther. 2002;1(1):76–82.
- Silver JK, Gilchrist LS. “Cancer rehabilitation with a focus on evidence-based outpatient physical and occupational therapy interventions.” American Journal of Physical Medicine & Rehabilitation, 2011;90(5):S5-S15.
- Stone PC, Minton O. Cancer-related fatigue. Eur J Cancer. 2008; 44(8):1097–1104.