Understanding arthritis and joint health is not purely an academic exercise; it’s a critical life skill that can affect your daily routine, productivity, and overall wellbeing. Arthritis, often dismissed as a condition of old age, can strike at any stage of life, undermining your capacity to perform simple tasks like opening a jar or walking your dog.
Consider arthritis as a ‘roadblock’ on the highway of life. Just as a roadblock causes congestion and delays, arthritis disrupts the smooth flow of movement, causing pain and limiting mobility. The stakes are high; failing to navigate this roadblock effectively can reduce quality of life.
This post is your ‘roadmap’ for understanding arthritis and joint health. We’ll examine its impact on daily life, explore various treatment options, and offer preventative strategies. Real-world examples and evidence-based recommendations will punctuate the discussion, providing a holistic view of managing arthritis across multiple joints.
The Impact of Understanding Arthritis and Joint Health on Daily Life
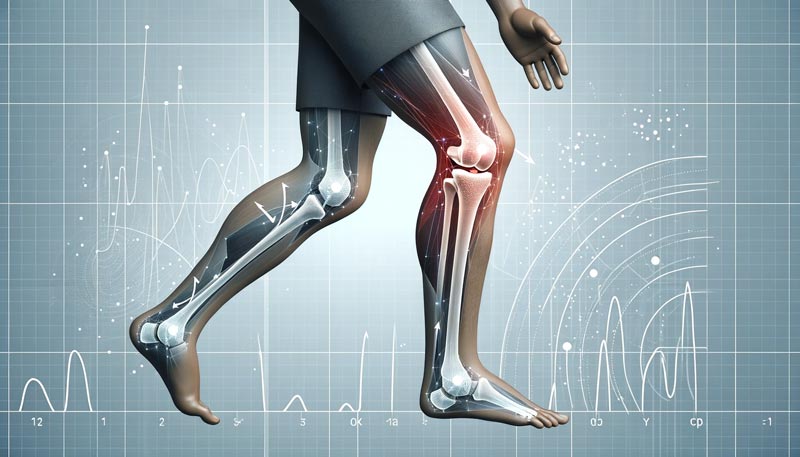
The repercussions of arthritis are far-reaching, affecting the individual and their ability to engage in daily activities. Understanding Arthritis and Joint Health is crucial, especially when knee osteoarthritis can significantly alter weight-bearing exercises, including walking and standing. This is corroborated by studies showing that individuals with Osteoarthritis (OA) display different joint kinetics at the knee compared to those without the condition.
Furthermore, OA impacts gait patterns, leading to increased knee adduction and decreased knee flexion movements. This is not merely a biomechanical issue; it’s a life-altering problem that can limit mobility and independence. Gender-specific differences in gait biomechanics have also been observed, suggesting that treatment interventions should be tailored based on gender.
Chronic hip pain, another manifestation of arthritis, can be exacerbated by muscle imbalances, such as weakness in the gluteus maximus and medius. This highlights the importance of understanding arthritis and joint health, as it can inform more effective treatment strategies.
A nuanced understanding of arthritis is crucial for managing its impact on daily life. From altering gait patterns to affecting the ability to perform weight-bearing activities, arthritis can be a significant barrier to maintaining a healthy lifestyle. Therefore, evidence-based approaches to managing the condition are essential for improving quality of life.
Treatment Options for Various Forms of Arthritis
Pharmaceutical treatments for arthritis vary widely. Analgesics, glucocorticoids, and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used. For Rheumatoid Arthritis (RA), disease-modifying antirheumatic drugs (DMARDs) are often prescribed.
OA treatment typically starts with acetaminophen for mild symptoms and oral NSAIDs for moderate ones. NSAIDs, however, carry risks such as gastrointestinal issues and renal complications. Intra-articular corticosteroid injections and viscosupplementation with hyaluronic acid offer short-term relief for knee OA.
In understanding arthritis and joint health, RA treatments aim to suppress inflammatory cytokines and reduce immune system overactivity. Medications like methotrexate and biologic agents targeting specific inflammatory cytokines offer a more targeted approach.
Acetaminophen is often recommended for mild to moderate arthritis pain. Still, it comes with risks like potential liver damage and gastrointestinal bleeding. Prescription anti-inflammatories like naproxen sodium can also raise blood pressure and cause lower extremity swelling.
For systemic forms of arthritis, DMARDs, glucocorticoids, or biologic drugs are often prescribed. These medications are effective for pain relief and slowing joint deterioration but come with risks like liver and kidney damage.
In understanding arthritis and joint health, exercise is a compelling alternative to pharmaceutical solutions. Exercise improves joint function and mitigates pain without the side effects associated with medications. Tailored exercise regimes can offer a more sustainable and holistic approach to managing arthritis.

How Understanding Arthritis and Joint Health Affects Multiple Joints
RA often initiates its degenerative course in smaller joints, such as the hands and feet, before progressing to larger joints, like the knees and hips. This progression pattern underscores the importance of early diagnosis and intervention. Timely treatment can alleviate symptoms in the initially affected joints and prevent or delay the disease from wreaking havoc on multiple joints, thereby preserving overall mobility and quality of life.
The strength of the quadriceps muscle is a significant factor in the onset and progression of knee OA. A strong quadriceps muscle reduces the risk of developing knee OA by 64%, serving as a protective mechanism. This isn’t just about the knee; the quadriceps also influence the hip joint. Therefore, a targeted muscle-strengthening program can be a multi-joint defensive strategy, offering benefits beyond a single joint.
Systemic forms of arthritis, such as RA, can have far-reaching effects beyond the joints, manifesting in symptoms like lung inflammation, pericarditis, and even osteoporosis. Recognising these systemic effects is crucial for developing comprehensive treatment plans. A multi-joint and multi-system approach to treatment becomes indispensable, ensuring that all affected areas receive attention.
Total hip replacement is often the last resort for severe arthritis cases. It can result in a significant loss of strength, up to 80%, even two years after the operation. This long-term impacts both the hip and adjacent joints like the knee. Understanding this can guide healthcare providers in developing a more holistic, long-term approach to arthritis management, which may include pre- and post-operative physical therapy to mitigate these effects.
In the broader scope of understanding arthritis and joint health, adopting a multi-joint perspective is not just beneficial—it’s essential. This comprehensive view can guide more effective, personalised treatment strategies, including incorporating exercise as a viable alternative to medication.
Exercise Regimens for Arthritis Management Across Joints
Arthritis is a multifaceted challenge that extends well beyond medication. Exercise is a cornerstone in this intricate landscape, offering a nuanced approach to managing arthritis effectively.
The type, intensity, and frequency of exercise are not mere variables but pivotal factors that can alleviate or exacerbate arthritis symptoms. Customising these elements to individual needs can result in a marked improvement in quality of life, reduced pain, and enhanced functional mobility.
Another crucial point in understanding arthritis and joint health is that exercise for arthritis isn’t a one-size-fits-all solution. Different forms of arthritis require tailored exercise programmes. For instance, OA may benefit more from weight-bearing exercises, while RA might require a different approach. The key is to consult healthcare providers for a tailored exercise plan, which can be a game-changer in managing arthritis symptoms and improving overall wellbeing.
There are specific types of exercises that are beneficial for managing arthritis. Each category of exercise serves a unique purpose. Understanding these can empower individuals to make informed decisions for a holistic approach to arthritis management.

1. Aerobic Exercise
In understanding arthritis and joint health, aerobic fitness is often compromised in arthritis patients. Land-based aerobic training has shown moderate effects on aerobic capacity, pain, and quality of life.
For those with RA, combined aerobic and resistance training has shown positive effects on cardiovascular disease (CVD) risk factors. If walking is difficult, biking is an excellent alternative. Aquatic activities are also an option but offer less cardiovascular benefit.
2. Resistance Training
Resistance training is vital for joint protection. Programs range from 15 to 60 minutes, 2–7 days per week, for 3–104 weeks. The load ranges from 30% to 100% of 1-RM (1 repetition maximum). Specific exercises like chair squats and knee extension machines target key muscle groups, aiding in daily activities like walking and stair climbing.
3. Flexibility
Stretching is essential but should be done cautiously. Techniques include static and dynamic stretching. You should never hold a stretch that causes increased pain. Flexibility exercises target the hamstrings, gastrocnemius, and soleus, aiding in functional mobility.
4. Neuromotor Training
Tai chi and yoga are excellent for neuromotor training. They improve joint proprioception and offer the added benefit of relaxation. A more frequent program of five to seven days per week is beneficial.
After discussing the importance of aerobic, resistance, flexibility, and neuromotor training, it’s crucial to look at specific exercises that can be incorporated into your daily routine.
These exercises are not randomly selected; they are meticulously chosen to target specific muscle groups essential for daily activities. They are the building blocks for a comprehensive exercise programme tailored to arthritis management.
- Total Gym: Targets gluteal muscles, quadriceps, and hamstrings. Helps with: Sit-to-stand, stairs, walking dog, walking speed.
- Chair Squat: You may add a backpack with weights for resistance. Involves the gluteal maximus, quadriceps, and hamstrings. Helps with: Sit-to-stand, stairs, walking dog, walking speed.
- Knee Extension Machine: May work within a pain-free range. Targets quadriceps. Helps with: Sit-to-stand, stairs, walking dog, walking speed.
- Hamstring Curl: May work within a pain-free range. Targets hamstrings. Helps with Stairs, walking dog, and walking speed.
- Shoulder Press Machine: Use the front grip option to avoid shoulder pain. Works deltoids triceps. Helps with Pushing and reaching overhead.
- Seated Rows: Maintain scapular retraction and lumbar lordosis. Works latissimus dorsi, rhomboids, middle trapezius. Helps with Control dog leash and lifting groceries.
- Grip Strengthening with Therapy Putty: Use progressively resistant putty. Targets finger flexors. Helps with opening jars and carrying groceries.
- Finger Adduction with Putty: Use progressively resistant putty. Works finger adductors. Helps with opening jars and carrying groceries.
- Brisk Walking: On flat terrain or in water at waist level. Targets gluteals, hamstrings, quadriceps. Helps with walking endurance and lower extremity muscle performance.
- Flexibility Exercises: Avoid ballistic movements. It targets hamstrings, gastrocnemius, and soleus. Helps with functional mobility for stairs, walking, and squatting.
In understanding arthritis and joint health, it’s clear that exercise plays a significant role. The exercise types, intensity, and frequency are not arbitrary choices but are deeply rooted in scientific evidence. Tailoring these to individual needs can make a significant difference in managing arthritis symptoms and enhancing the quality of life.
Understanding Arthritis and Joint Health: Preventative Measures
Arthritis prevention isn’t a secondary concern; it’s a strategic, evidence-based approach that can significantly alter the disease’s trajectory. A mere 10-pound weight loss can result in a substantial decrease in arthritis pain, highlighting the critical role of weight management. This section is a comprehensive guide looking at measures for understanding arthritis and joint health to mitigate the disease’s risks and symptoms.
The preventative measures discussed aren’t mere lifestyle adjustments but targeted interventions backed by scientific data. Strength training exercises, for example, have been linked explicitly to reduced cartilage loss and slower disease progression in osteoarthritis patients. These interventions aim to reduce joint stress and systemic inflammation, critical factors in arthritis onset and progression.
These measures aren’t a one-size-fits-all solution. They require individual tailoring. The following list offers a detailed breakdown of these preventative measures, each supported by scientific evidence, to guide your arthritis management strategy:
- Weight Management Through Exercise: A mere 10-pound weight loss can significantly alleviate arthritis pain.
- Regular Exercise for Joint Health: Exercise maintains joint health and lowers osteoarthritis risk, with strength training offering particular benefits.
- Footwear and Orthotics: Quality athletic shoes and custom orthotics can correct biomechanical issues, reducing joint stress.
- Joint Protection Techniques: Using stronger joints for strenuous tasks can mitigate everyday stress.
- Smoking Cessation: Quitting smoking reduces the severity and progression of rheumatoid arthritis.
- Medication and Supplement Cautions: Some medications, like NSAIDs, can accelerate joint degeneration, elevating OA risk.

The Importance of Proprioception in Arthritis Management
Proprioception, the sense of body position, is a critical but often overlooked factor in understanding arthritis and joint health, especially in knee OA. Research shows that a loss of proprioception can worsen the arthritic process and contribute to impaired balance and postural control.
Mechanoreceptors in joint structures are essential for proprioception. When these receptors are damaged due to arthritis, proprioceptive acuity declines. This decline can lead to altered neuromuscular reflexes and joint loading patterns, accelerating cartilage breakdown.
Knee OA patients often exhibit poorer balance, postural control, and increased sway than healthy controls. This impairment is likely a result of both proprioceptive deficits and weakened muscle function around the joint. Furthermore, a decline in proprioceptive acuity has been observed in the knees, hips, and ankles.
Rehabilitation strategies focusing on balance, proprioceptive, and neuromuscular training are promising for reducing sway, improving stability, and decreasing fall risk. Tai chi is particularly effective in enhancing proprioceptive ability and postural control. Additionally, external supports like elastic knee bandages can increase proprioceptive ability by up to 40%, offering valuable feedback.
Patients with knee OA also show altered muscle activation patterns and balance and gait impairments. Neuromotor training that challenges dynamic balance is a crucial component of arthritis management. Comprehensive therapy to restore proprioception, strength, range of motion, and neuromuscular control can offer significant functional improvements.

Final Thoughts on Understanding Arthritis and Joint Health
Understanding arthritis and joint health is a complex but vital issue with far-reaching implications for our daily lives, overall wellness, and long-term health outcomes. This post has examined the multi-dimensional nature of arthritis, spanning its impact on daily activities, the available treatment options, and the importance of early diagnosis and personalised treatment plans.
In light of recent findings, it’s abundantly clear that exercise isn’t just an auxiliary component but a central pillar in treating and preventing arthritis. A balanced exercise programme, tailored to individual needs and disease severity, offers many benefits without exacerbating joint damage. Exercise promotes joint health, alleviates pain, and is a preventive measure against degenerative changes.
Beyond exercise, other lifestyle measures like weight management and smoking cessation can significantly alter the trajectory of the disease. Implementing a comprehensive strategy that includes these elements and judicious pharmacological management can yield optimal control over arthritis, enhancing the quality of life.
As we look forward, the horizon appears promising. Ongoing research aims to refine exercise prescription guidelines for specific subpopulations and explore new rehabilitation methods. These advancements and the development of supportive devices and pharmacological treatments will further empower individuals to manage arthritis effectively.
Fundamentally, understanding arthritis and joint health is not a matter for healthcare providers; it’s a societal imperative. As the global population ages, a proactive approach rooted in lifestyle changes and community support becomes increasingly crucial. Armed with the proper knowledge, tools, and strategies, we can combat arthritis more effectively, making it less of a ‘roadblock’ and more manageable.
Sources
- Baillet, A., Vaillant, M., Guinot, M., Juvin, R., Gaudin, P. 2012. Efficacy of resistance exercises in rheumatoid arthritis: meta-analysis of randomized controlled trials. Rheumatology (Oxford). Mar;51(3):519-27.
- Baillet, A., Zeboulon, N., Gossec, L., et al. 2010. Efficacy of cardiorespiratory aerobic exercise in rheumatoid arthritis: meta-analysis of randomized controlled trials. Arthritis Care Res. Jul;62(7):984-92.
- Barrett, D.S., Cobb, A.G., Bentley, G. 1991. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. Jan;73(1):53-6.
- Buckwalter, J.A., Martin, J. 2006. Osteoarthritis. Adv Drug Deliv Rev. Nov 10;58(2):150-67.
- Costenbader, K.H., Feskanich, D., Mandl, L.A., Karlson, E.W. 2004. Smoking intensity, duration, and cessation, and the risk of rheumatoid arthritis in women. Am J Med. Jun 15;116(6):350-7.
- de Jong, Z., Munneke, M., Zwinderman, A.H., et al. 2003. Is a long-term high-intensity exercise program effective and safe in patients with rheumatoid arthritis? Results of a randomized controlled trial. Arthritis Rheum. Sep;48(9):2415-24.
- Durcan, L., Wilson, F., Cunnane, G. 2014. The effect of exercise on sleep and fatigue in rheumatoid arthritis: a randomized controlled study. J Rheumatol. Oct;41(10):1966-73.
- Firestein, G.S. 2003. Evolving concepts of rheumatoid arthritis. Nature. May 15;423(6937):356-61.
- Flint-Wagner, H.G., Lisse, J., Lohman, T.G., et al. 2009. Assessment of a sixteen-week training program on strength, pain, and function in rheumatoid arthritis patients. J Clin Rheumatol. Jun;15(4):165-71.
- Gibofsky, A. 2012. Overview of epidemiology, pathophysiology, and diagnosis of rheumatoid arthritis. Am J Manag Care. Dec;18(13 Suppl):S295-302.
- Häkkinen, A. 2004. Effectiveness and safety of strength training in rheumatoid arthritis. Curr Opin Rheumatol. Mar;16(2):132-7.
- Hassan, B.S., Mockett, S., Doherty, M. 2001. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis. Jun;60(6):612-8.
- Hochberg, M.C. 2001. Pharmacological therapy of osteoarthritis. Best Pract Res Clin Rheumatol. Oct;15(5):583-92.
- Hochberg, M.C., Altman, R.D., April, K.T., et al. 2012. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). Apr;64(4):465-74.
- Hootman, J.M., Fitzgerald, S., Macera, C., Blair, S.N. 2004. Lower extremity muscle strength and risk of self-reported hip or knee osteoarthritis. J Phys Act Health. Jul;1:321-30.
- Hurwitz, D.E., Sumner, D.R., Andriacchi, T.P., Sugar, D.A. 1998. Dynamic knee loads during gait predict proximal tibial bone distribution. J Biomech. May;31(5):423-30.
- Kaufman, K.R., Hughes, C., Morrey, B.F., Morrey, M., An, K. 2001. Gait characteristics of patients with knee osteoarthritis. J Biomech. Jul;34(7):907-15.
- Lane, N.E., Oehlert, J.W., Bloch, D.A., Fries, J.F. 1998. The relationship of running to osteoarthritis of the knee and hip and bone mineral density of the lumbar spine: a 9 year longitudinal study. J Rheumatol. Feb;25(2):334-41.
- Lewis CL, Sahrmann SA. Muscle activation and movement patterns during prone hip extension exercise in women. J Athl Train. 2009 May-Jun;44(3):238-48.
- Leong, D.J., Sun, H.B. 2014. Osteoarthritis – why exercise? J Exerc Sports Orthop. 2014;1(1):04.
- McKean, K.A., Landry, S.C., Hubley-Kozey, C.L., et al. 2007. Gender differences exist in osteoarthritic gait. Clin Biomech (Bristol, Avon). Jun;22(5):400-9.
- Messier, S.P. 2006. Arthritic diseases and conditions. In: Kaminsky, L.A., editor. ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription. 5th ed. Baltimore (MD): Lippincott Williams & Wilkins. p. 500-13.
- Miller TD, Squires RW, Gau GT, Ilstrup DM, Frohnert PP, Sterioff S. Graded exercise testing and training after renal transplantation: a preliminary study. Mayo Clin Proc. 1987 Sep;62(9):773-7
- Miyazaki, T., Wada, M., Kawahara, H., et al. 2002. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. Jul;61(7):617-22.
- Nallegowda, M., Singh, U., Bhan, S., et al. 2003. Balance and gait in total hip replacement: a pilot study. Am J Phys Med Rehabil. Sep;82(9):669-77.
- Roddy, E., Zhang, W., Doherty, M. 2005. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis. Apr;64(4):544-8
- Stavropoulos-Kalinoglou, A., Metsios, G.S., Veldhuijzen van Zanten, J.J., et al. 2013. Individualised aerobic and resistance exercise training improves cardiorespiratory fitness and reduces cardiovascular risk in patients with rheumatoid arthritis. Ann Rheum Dis. Nov;72(11):1819-25.
- Westhoff, G., Rau, R., Zink, A. 2008. Rheumatoid arthritis patients who smoke have a higher need for DMARDs and feel worse, but they do not have more joint damage than non-smokers of the same serological group. Rheumatology (Oxford). Jun;47(6):849-54.
- Zhang, Y., Jordan, J.M. 2010. Epidemiology of osteoarthritis. Clin Geriatr Med. Aug;26(3):355-69.



