Your flexibility limits affect how well you can move and stretch. Many fitness enthusiasts reach a point where their range of motion seems to hit an immovable wall. This stems from how different bodily structures work together through biotensegrity (a biological structure consisting of continuously connected tension and discontinuous compression elements).
Our bodies operate through a network where bones act as compression elements within an organised tension framework from connective tissues. This arrangement means movement restrictions arise from various sources, not just tight muscles.
The fascial system (connective tissue that wraps around muscles and organs) serves a vital role. It contains collagen fibres and a hydrated extracellular matrix (a gel-like substance between cells providing structural support and nutrients) influencing our movement capabilities.
Muscles and bones form just one part of what creates flexibility limits. Research shows that neural tissue must move freely between surrounding structures to accommodate various forces during movement. This interaction explains why some stretching plateaus occur despite dedicated practice.
Scientific evidence reveals that range of motion improvements happen through several pathways. These include changes in tissue mechanics and alterations in stretch tolerance. However, certain anatomical features set firm boundaries that no stretching can overcome.
The sections ahead detail the distinctions between muscle tension and bone compression. You’ll discover practical ways to identify these limitations, and we’ll examine how to work effectively with your body’s natural architecture.
What Causes Tension and Compression
The human body implements a sophisticated tensegrity system to control movement and maintain stability. This system affects flexibility limits through a continuous tension and compression forces network.
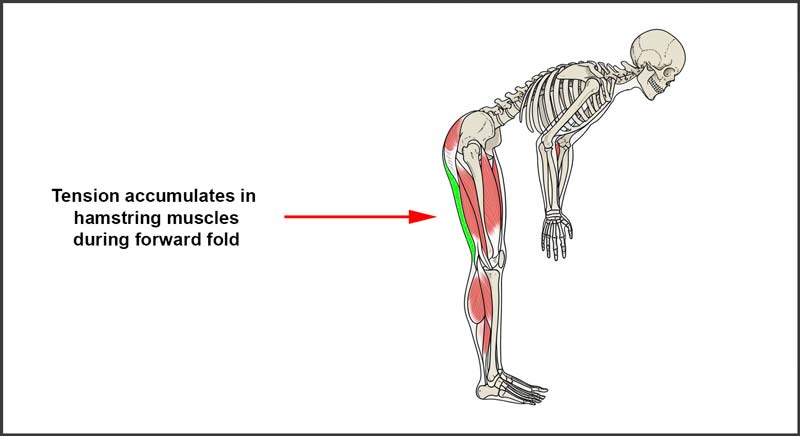
Muscle tension occurs when muscles, ligaments, tendons, and fascia lengthen to their current capacity. The fascia (connective tissue) creates a dynamic linking system that transmits force through muscles and creates natural pretension.
Sensory nerve fibres within the fascia respond to pressure and movement. These neural responses directly influence your flexibility limits by triggering protective responses when tissues stretch too quickly or far.
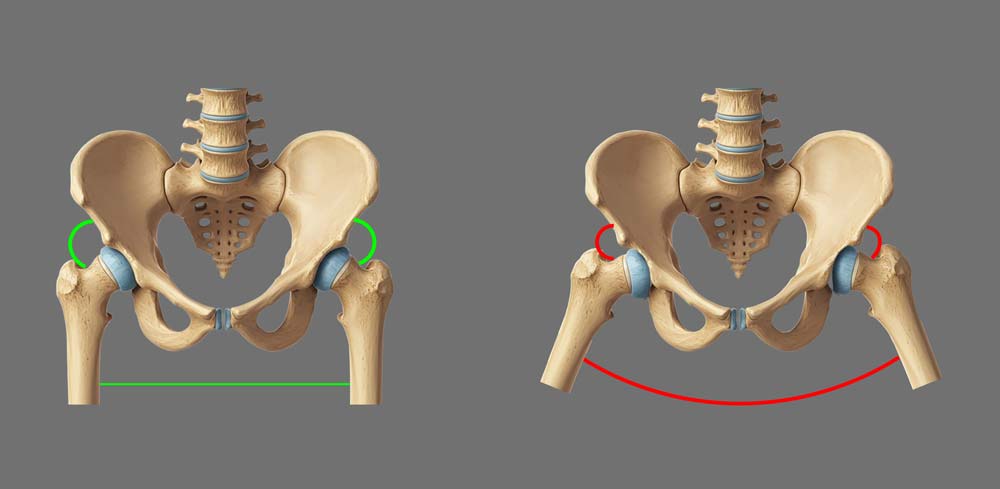
Bone compression presents a different type of restriction. When bones meet during movement, they create a firm endpoint that no amount of stretching can change. This compression happens at the opposite side of where you feel the stretch.
Your individual anatomy determines where and when bone compression occurs. Factors include the length of bony processes (protrusions), joint structure, and the thickness of cartilage surfaces.
How to Identify Your Flexibility Limits
Recognising whether muscle tension or bone compression limits your movement requires attention to specific sensations. Your body creates distinct signals for flexibility limits based on the restricting factor.
Muscle tension presents as a stretching sensation in the lengthening tissues. This feeling occurs on the same side as the stretching muscles. For example, when touching your toes, you feel tension in the back of your legs.
Bone compression creates a firm blocking sensation. This stopping point feels solid and appears on the opposite side of the stretch. Compression might occur at the front of your hip joints during a forward bend.
The table below outlines the key differences between tension and compression sensations:
| Characteristic | Muscle Tension | Bone Compression |
|---|---|---|
| Location | Same side as stretch | Opposite side of stretch |
| Sensation | Stretching, pulling feeling | Firm, solid blocking |
| Response to continued stretching | Can gradually yield | Remains fixed |
| Feel on pressure | Soft tissue gives | Hard endpoint |
Several factors influence where you experience these flexibility limits. Genetics affect tissue elasticity, while body proportions determine how movements feel. Women typically show a greater range of motion at hips, knees, and ankles than men.
Testing for compression requires careful attention to positioning. When examining a joint’s range, move slowly and note where you feel resistance. The sensation’s location and quality reveal whether you’ve reached a tissue tension limit or a bony endpoint.
Testing Different Body Parts
Your musculoskeletal system creates distinct flexibility limits at different joints. Based on its anatomical structure, each area presents unique tension and compression patterns.
The testing process requires careful attention to both sensation and position. Moving slowly through each range helps identify where actual restrictions occur. Your flexibility limits might vary between the left and right sides.
Spine and Back
The spinal column shows varying compression points based on individual vertebral structures. The spinous processes (bony tips along your spine) determine how far you can bend backwards. Their length and thickness vary between vertebrae and between individuals.
During back bends tension appears in your abdomen and hip flexors. As you progress, you might feel compression where vertebrae meet. This compression point often differs between people – some feel it in their lower back, others in their mid-back region.
Hip Joint
Hip flexibility involves a complex interaction between the femur (thigh bone) and pelvis. When lying on your back with your legs up against a wall, tension typically appears in the adductor muscles (inner thigh). Compression occurs where the femur meets the pelvis.
The hip socket’s depth and orientation affect where compression happens. Some people reach compression earlier on one side due to subtle differences in hip socket position or femur shape.
Knee Complex
Knee flexibility primarily shows tension patterns in the surrounding muscles. The joint’s hinge-like structure means compression rarely limits normal range. However, the knee cap (patella) can create compression during deep flexion.
Shoulder Region
Shoulder mobility combines movements from multiple joints. The shoulder blade’s position on your rib cage affects where compression occurs. Tension patterns appear in the chest muscles and rotator cuff, while compression might occur between bones during extreme positions.

Working Within Your Natural Flexibility Limits
Each person’s body presents unique anatomical features that influence their range of motion. Genetic factors affect tissue elasticity and flexibility limits, while body proportions determine movement patterns.
Your muscles respond to stretching through mechanotransduction (converting mechanical forces into cellular responses). This process allows tissues to adapt gradually when you work within appropriate ranges.
The fascial system creates a continuous network throughout your body. This connective tissue contains various sensory fibres that respond to pressure and movement. These responses help regulate your safe range of motion.
Body temperature affects tissue pliability. Cold muscles contract in response to quick or aggressive stretching, creating the opposite effect of lengthening. The fascia system requires proper warming to respond optimally to stretch.
Several key principles govern safe flexibility training:
- Move slowly through ranges to avoid triggering protective muscle contractions
- Hold positions for 20-60 seconds to allow proper tissue adaptation
- Use slow, nasal breathing to promote the parasympathetic response
- Exit stretches gradually to protect spinal structures
- Ensure muscles are appropriately warmed before stretching
- Stay within ranges that feel comfortable and controlled
- Compare sensations between the left and right sides
Your individual anatomical structure determines your movement possibilities. Broader shoulders might affect specific stretches, while leg-to-torso proportions influence how movements feel.
The fascia’s response to manual pressure varies between individuals. Its composition of collagen fibres and hydrated extracellular matrix creates unique movement signatures in each person.
Physical characteristics create your personal movement blueprint. These natural boundaries shape how you move through space and respond to different positions.
Sources
- Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function — part 1. N Am J Sports Phys Ther. 2006;1(3):132–9.
- de Ridder R, De Blaiser C, Verrelst R, De Saer R, Desmet A, Schuermans J. Neurodynamic sliders promote flexibility in tight hamstring syndrome. Eur J Sport Sci. 2020;20: 973–980.
- Doriot N, Wang X. Effects of age and gender on maximum voluntary range of motion of the upper body joints. Ergonomics. 2006;49(3):269-281.
- Christmas C, Andersen RA. Exercise and older patients: guidelines for the clinician. J Am Geriatr Soc. 2000;48(3):318-324.
- Herda T.J., Herda N.D., Costa P.B., Walter-Herda A.A., Valdez A.M., and Cramer J.T. 2013. The effects of dynamic stretching on the passive properties of the muscle-tendon unit. J. Sports Sci. 31: 479–487.
- Magnusson S.P., Simonsen E.B., Aagaard P., Dyhre-Poulsen P., McHugh M.P., and Kjaer M. 1996a. Mechanical and physical responses to stretching with and without preisometric contraction in human skeletal muscle. Arch. Phys. Med. Rehabil. 77: 373–378.
- Mitchell U.H., Myrer J.W., Hopkins J.T., Hunter I., Feland J.B., and Hilton S.C. 2007. Acute stretch perception alteration contributes to the success of the PNF “contract-relax” stretch. J. Sport Rehabil. 16: 85–92.
- Nee RJ, Butler D. Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport. 2006;7: 36–49.
- Norkin CC, Levangie PK. Joint Structure and Function: A Comprehensive Analysis. 5th ed. Philadelphia (PA): F.A. Davis; 2011. 588 p.
- Pardehshenas H, Maroufi N, Sanjari MA, Parnianpour M, Levin SM. Lumbopelvic muscle activation patterns in three stances under graded loading conditions: Proposing a tensegrity model for load transfer through the sacroiliac joints. J Bodyw Mov Ther. 2014 Oct;18(4):633-42.
- Shin G, Shu Y, Li Z, Jiang Z, Mirka G. Influence of knee angle and individual flexibility on the flexion-relaxation response of the low back musculature. J Electromyogr Kinesiol. 2004;14(4):485-494.
- Silva A, Manso A, Andrade R, Domingues V, Brandão MP, Silva AG. Quantitative in vivo longitudinal nerve excursion and strain in response to joint movement: A systematic literature review. Clin Biomech (Bristol, Avon). 2014;29: 839–847.
- Willard FH, Vleeming A, Schuenke MD, Danneels L, Schleip R. The thoracolumbar fascia: anatomy, function and clinical considerations. J Anat. 2012 Dec;221(6):507-36.
- Zügel M, Maganaris CN, Wilke J, et al. Fascial tissue research in sports medicine: from molecules to tissue adaptation, injury and diagnostics: consensus statement. Br J Sports Med. 2018 Dec;52(23):1497.



