By BeSund Editorial Team 11/07/2023 Modified Date: 07/11/2024
Sleep
Learn how exercise can influence sleep quality
Sleep and Restorative Health
Understanding Sleep and Restorative Health Fundamentals
Sleep and restorative health demonstrate a fundamental evolutionary adaptation, emerging over 500 million years ago during the Cambrian explosion. This biological necessity manifests across every studied animal species, from primitive worms to complex mammals, highlighting its critical role in sustaining life.
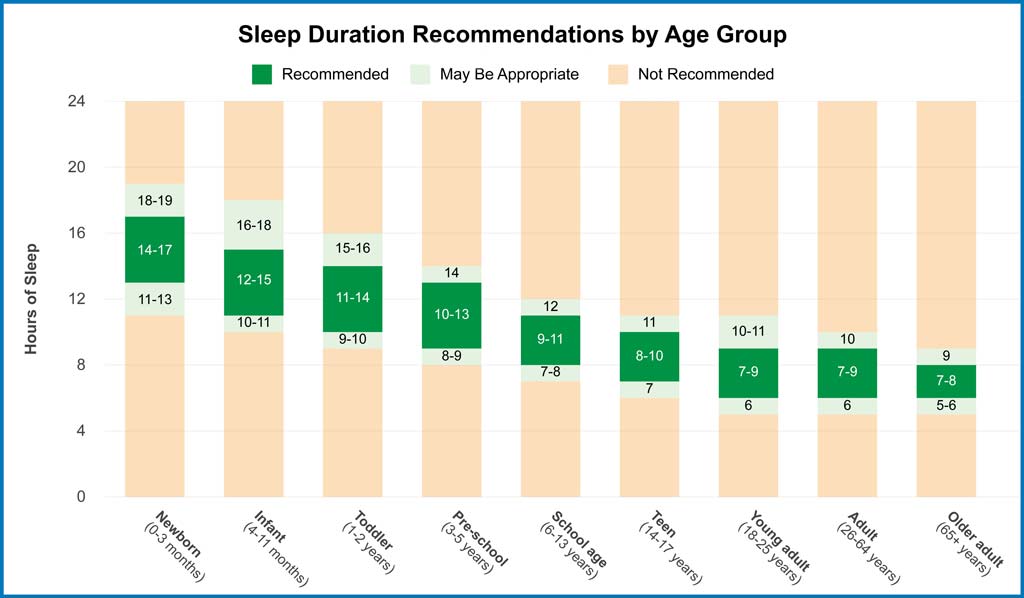
Throughout life, optimal sleep and restorative health requirements vary significantly. Humans require 7-8 consecutive hours to maintain vital functions.
Scientific understanding has evolved beyond viewing sleep as a passive state of unconsciousness. Research reveals that sleep is an intensely metabolically active process essential for survival, with specific brain regions exhibiting up to 30% increased activity compared to wakefulness.
The brain undergoes unique psychotic-like experiences during sleep, including hallucinations and memory alterations, which serve as normal biological processes crucial for cognitive function.
The comprehensive sleep duration recommendations chart below illustrates the dynamic nature of sleep requirements across different life stages. These evidence-based guidelines reflect the complex interplay between age-related developmental needs and essential restorative processes. Moreover, sleep timing proves equally crucial, with the initial four-hour window between 10:00 p.m. and 2:00 a.m. providing vital restorative benefits.
Investigations into sleep and restorative health mechanisms reveal complex neural processes involving multiple neurotransmitter systems. These include serotonin for mood regulation, adenosine for sleep promotion, and melatonin for circadian rhythm maintenance. These complex mechanisms prove essential for appreciating sleep’s role in maintaining optimal health.
The Architecture of Sleep
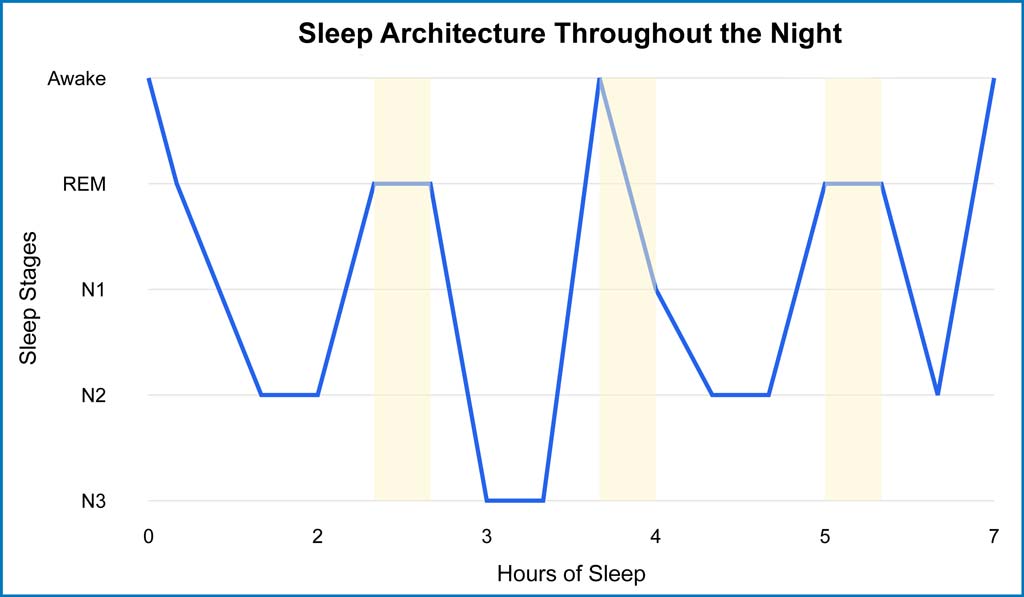
Sleep architecture comprises distinct states of brain activity, primarily categorised into non-rapid eye movement (NREM) and rapid eye movement (REM) sleep.
Each cycle between these states typically lasts 90-120 minutes, with NREM sleep dominating the first half of the night and REM sleep becoming more prevalent later. This precise orchestration of sleep and restorative health patterns ensures optimal cognitive and physical recovery.
During NREM sleep, the brain progresses through three distinct stages. Stage N1, the initial transition phase, involves decreased body temperature and muscle relaxation. Stage N2 marks the onset of proper sleep, characterised by distinctive brain patterns called sleep spindles. Stage N3, known as deep sleep, features significantly reduced blood pressure and pulse rates.
REM sleep introduces a paradoxical state where, despite physical paralysis, the brain exhibits intense activity. During this phase, sleep and restorative health processes focus on emotional regulation and memory consolidation. Blood pressure increases while heart rate and breathing accelerate to daytime levels, with most dreaming occurring during this stage.
Below, the sleep architecture hypnogram illustrates the dynamic transitions between sleep stages across a typical night. The downward progression on the y-axis represents deeper sleep states, from wakefulness through light sleep (N1, N2) to deep sleep (N3), with REM periods highlighted.
This scientific visualisation reveals how the brain cycles through these stages roughly every 90 minutes, with deeper sleep dominating early hours and REM sleep becoming more frequent toward morning. The pattern demonstrates sleep and restorative health’s intricate orchestration throughout the night.
Sleep and Restorative Health Mechanisms
Sleep drives critical cellular repair processes throughout the brain and body, with studies revealing complex neurochemical changes that facilitate restoration. During this time, sleep and restorative health processes activate the brain’s glymphatic system, increasing its cleaning efficiency by 10-20 times compared to wakefulness.
The brain demonstrates remarkable plasticity during sleep phases, with specific regions becoming highly active in coordinated patterns. Growth hormone, which surges during sleep, initiates crucial vascular repair processes while maintaining blood vessel integrity. Additionally, the complete cessation of stress-related chemicals, such as noradrenaline, occurs exclusively during specific sleep phases.
Multiple immune-related substances, traditionally viewed within the innate immune system, actively regulate sleep-wake behaviour. These mechanisms involve an elaborate biochemical network comprising cytokines, chemokines, and growth factors. This sophisticated relationship between sleep and restorative health processes significantly influences cellular repair and immune system maintenance.
Sleep’s Role in Restorative Processes
Sleep and restorative health demonstrate powerful effects on immunological memory, substantially enhancing the body’s capacity to recognise and respond to antigens. Studies indicate that individuals receiving vaccinations after seven or more hours of sleep develop twice the antibody response compared to those with insufficient rest.
The restoration process benefits the immune function, protein synthesis and tissue repair. Research examining sleep deprivation’s impact reveals concerning effects, including deterioration of skin integrity, internal organ compromise, and significant changes in vital organs. Furthermore, sleep and restorative health processes regulate core body temperature and metabolic function.
Sleep facilitates crucial synaptic repair and maintenance processes that counteract arousal’s toxic effects. The neurochemical environment during sleep presents vital windows for cellular homeostasis restoration, increasing signal-to-noise ratios and reinforcing neuronal circuitry. These processes prove especially active during the initial four-hour sleep window when the body prioritises repaying sleep debt and neutralising fatigue.
The Impact of Sleep on Health and Longevity
The long-term impact of sleep and restorative health manifests through mortality patterns revealed in epidemiological research. Studies tracking over five million subjects demonstrate that insufficient and excessive sleep durations correlate significantly with shortened lifespans through distinct biological mechanisms.
Meta-analyses spanning six continents consistently reveal a U-shaped mortality curve, where individuals sleeping less than seven hours show a 12% greater risk of death, whilst those exceeding nine hours demonstrate a 30% increased mortality risk.
Moreover, sleep and restorative health patterns are particularly significant for older populations, with prolonged sleep durations showing stronger mortality associations in East Asian demographics than in European and American populations.
Analysis of mortality data spanning 1950 to 2021 illuminates profound shifts in global health outcomes related to sleep duration. While overall mortality figures have shown variations, cardiovascular-related deaths linked to sleep patterns have increased to approximately 6.12 million annually, reflecting escalating challenges in maintaining optimal sleep duration.
Physical Health Consequences of Sleep Deprivation
Research examining sleep and restorative health reveals severe cardiovascular implications of sleep deprivation.
Studies across eight countries demonstrate that progressively shorter sleep correlates with a 45% increased risk of coronary heart disease development or mortality within 7-25 years. Japanese research indicates that workers who sleep six hours or less face a 400-500% higher risk of cardiac events over fourteen years.
Sleep loss triggers complex metabolic disruptions through multiple pathways. After just six nights of four-hour sleep, the body’s glucose processing efficiency decreases by 40%, creating pre-diabetic conditions. Sleep deprivation also alters metabolic hormones, specifically increasing ghrelin and reducing leptin levels, significantly impacting appetite regulation.
Laboratory findings demonstrate that chronic sleep restriction leads to widespread physical deterioration. Studies showed that sleep-deprived rats experienced extensive physiological damage within two to three weeks, revealing compromised temperature regulation, metabolic disruption, and immune system failure.
Furthermore, research indicates that even one night of four-hour sleep reduces natural killer cell activity by 70%, critically impairing the body’s ability to fight cancer and other diseases.
Poor sleep patterns significantly impact physiological recovery and healing mechanisms. Joint pain upon waking often indicates insufficient sleep over several consecutive days, as sleep helps reduce inflammation.
Sleep’s Role in Mental and Cognitive Function
Sleep and restorative health significantly influence memory formation and cognitive processing. Research demonstrates that sleep before learning refreshes the brain’s ability to form new memories, with the hippocampus acting as a temporary storage site that requires regular clearing through quality sleep.
Brain imaging studies reveal the profound impacts of sleep deprivation on emotional regulation. The amygdala, responsible for processing emotions like anger and rage, becomes 60% more reactive when sleep-deprived. Meanwhile, the prefrontal cortex’s ability to control these emotional responses diminishes significantly, leading to heightened emotional instability.
Studies examining REM sleep’s impact show that 35-55% of emotional themes from daily experiences resurface during dreams, facilitating emotional processing and resolution.
Research from the 1960s demonstrated that selective REM sleep deprivation, while allowing NREM sleep, triggered psychological instability, including anxiety, mood changes, and hallucinations within just three days.

Sleep and Restorative Health Benefits for Longevity
The relationship between sleep and restorative health becomes increasingly crucial with age. Studies reveal that maintaining proper sleep patterns can reduce or delay the onset of Alzheimer’s disease by 5-10 years, highlighting sleep’s neuroprotective properties.
Research examining cellular ageing demonstrates that insufficient sleep damages telomeres – protective caps on chromosomes – in ways that mirror advanced ageing processes. Consequently, two individuals of identical chronological age may exhibit markedly different biological ages based on their sleep patterns.
Laboratory findings indicate that quality sleep provides significant protection against age-related cognitive decline. When individuals achieve optimal sleep duration, their brains demonstrate enhanced waste removal processes and repair mechanisms. Furthermore, individuals maintaining seven to eight hours of nightly sleep show superior maintenance of brain health throughout their lifespan.
Science of Sleep Cycles and Recovery
Molecular and cellular mechanisms controlling sleep and restorative health operate through sophisticated interactions between sleep timing and pressure (the body’s increasing need for rest during wakefulness).
Within each cell, daily cycles optimise essential functions through internal biological clocks that regulate energy acquisition, cellular protection, repair processes, and reproduction.
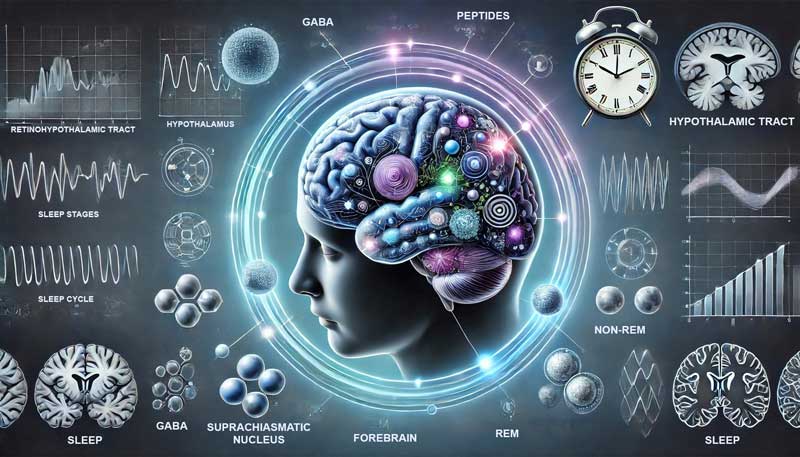
The brain’s master clock (suprachiasmatic nucleus) connects to other body systems using chemical signals: GABA (a calming brain chemical), peptides influencing blood vessels, and hormones regulating blood pressure. These pathways reach multiple brain regions, including the hypothalamus (which controls essential body functions), forebrain (responsible for complex thinking), and areas controlling sleep onset.
Special light-sensing cells in the retina transmit information about environmental light and darkness through a dedicated neural pathway (retinohypothalamic tract). Even minimal illumination of 8 lux (equivalent to dim twilight) proves capable of shifting sleep-wake patterns, with evening exposure to blue light particularly disruptive to natural sleep timing.
Sleep Stage Classifications and Functions
Advanced sleep and restorative health research reveals distinct mathematical models of sleep stage transitions, suggesting an abrupt shift between ages 2-3 years. This transition marks a change from neural reorganisation to facilitating neural repair processes.
Laboratory findings indicate significant variations in sleep architecture across different conditions. For example, stroke patients initially show minimal structural changes except for lengthened REM latency, whilst those with advanced conditions demonstrate shorter total sleep time and complex alterations in sleep stage distributions.
Studies examining oxygen requirements highlight how REM sleep demands higher metabolic and glucose levels than slow-wave sleep. This metabolic variation between sleep stages indicates specialised energy requirements for distinct restorative processes.
The Role of REM and Non-REM Sleep
Sleep and restorative health processes manifest differently during REM and non-REM phases, with research revealing their distinct functions. When deprived of deep sleep, individuals show decreased performance and significant recovery needs during subsequent rest.
The brain’s memory consolidation system suggests that electrical patterns in the hippocampus (the memory centre) coordinate with sleep-specific brain waves. This process transfers information from short-term storage to the neocortex (the brain’s outer layer) for long-term memory formation.
Research examining REM sleep patterns in developing children shows fascinating correlations with cognitive development. Higher amounts of REM sleep during preschool significantly enhance learned item retention, highlighting critical developmental windows.
Sleep and Restorative Health During Different Sleep Phases
Examining sleep and restorative health across different phases reveals complex neural activation patterns in posterior cerebral regions. Despite significant differences in subcortical neural activity, these patterns show remarkable similarities during REM and non-REM sleep.
The cyclic alternating pattern is an internal master clock that coordinates various physiological processes. This pattern maintains stability while enabling adaptive responses to internal and external stimuli throughout different sleep phases.
Laboratory findings demonstrate how sleep efficiency increases proportionally with total sleep duration. NREM stages and REM duration expand with increased total sleep time, though their relative distributions shift throughout the night.
Sleep and Restorative Health Disorders and Disruptions
Sleep disorders and disruptions are now a pervasive challenge across industrialised nations, affecting significant portions of the population and carrying major health consequences.
These disorders manifest through multiple pathways, affecting populations through approximately 80 distinct conditions. Clinical diagnostic criteria identify three primary categories: problems with sleep onset (difficulty falling asleep), sleep maintenance (difficulty staying asleep), and disorders affecting specific sleep stages.
The relationship between sleep and restorative health becomes particularly evident in clinical settings. Research reveals that fragmented sleep prevents achieving proper restoration, as the brain only registers actual sleep time rather than time spent in bed.
This fragmentation proves especially concerning as it correlates with increased arteriolosclerosis (hardening of small blood vessels) and subcortical macroscopic infarcts (small strokes in deeper brain tissue), serving as independent risk factors for cardiovascular disease.
Sleep disruption frequently precedes and potentially contributes to numerous psychiatric conditions. Studies indicate a bidirectional relationship between sleep and restorative processes in conditions including depression, anxiety, PTSD (Post-Traumatic Stress Disorder), schizophrenia, and bipolar disorder. This complicated connection demonstrates how sleep disruption can both signal and exacerbate mental health challenges.
Common Sleep Disorders and Their Impact
Insomnia represents the most prevalent sleep disorder, affecting approximately one-third of adults who report disrupted sleep patterns. Clinical studies reveal that about 10% experience severe symptoms causing significant daytime consequences, with women showing higher susceptibility (17.6% versus 10.1% in men).
Sleep apnoea, characterised by repeated breathing interruptions during sleep, presents unique challenges. Research indicates:
- The condition affects 2-4% of middle-aged adults
- Patients experience hundreds of breathing interruption events nightly
- These interruptions trigger automatic awakening responses
- Two-thirds of patients develop high blood pressure
- The condition significantly increases the risk of heart disease and stroke
Narcolepsy, affecting roughly 1 in 2,000 people, demonstrates how sleep and restorative processes become fundamentally disrupted. This condition stems from the loss of orexin-containing neurons in the hypothalamus, leading to:
- Abnormal transitions between wake and sleep states
- Sudden muscle control loss triggered by emotions (cataplexy)
- Sleep paralysis
- Dream-like hallucinations during wakefulness
- Disrupted nocturnal sleep patterns
Environmental and Lifestyle Sleep Disruptors
The impact of environmental factors on sleep and restorative health goes beyond individual habits. Research demonstrates that neighbourhoods characterised by high crime rates, lack of social cohesion, and poor maintenance correlate significantly with compromised sleep quality.
Temperature regulation plays a crucial role in maintaining restorative sleep patterns. Studies reveal:
- Optimal bedroom temperature centres around 18.3°C (65°F)
- Core body temperature must drop approximately 1°F to initiate sleep
- Late-night eating disrupts this cooling process by redirecting blood flow to digestion
- REM sleep shows particular sensitivity to temperature fluctuations due to minimal thermoregulatory ability during this stage
Hospital environments present unique challenges to sleep and restorative processes. Research indicates:
- Noise levels frequently match those of busy restaurants
- Patients receive minimal exposure to natural light (approximately 1.7 minutes daily)
- Constant artificial lighting disrupts circadian rhythms
- Regular disturbances contribute to ICU delirium, potentially leading to long-term cognitive dysfunction
Modern Technology and Sleep Quality
Digital technology profoundly impacts sleep and restorative health processes through multiple mechanisms. Studies reveal that 90% of people use electronic devices within an hour of bedtime, significantly disrupting natural sleep patterns.
Blue light exposure from electronic devices presents particular challenges to sleep architecture. Research demonstrates:
- Even dim light (8 lux) can suppress melatonin production
- Standard bedside lamps emit 20-80 lux
- Blue LED light has twice the melatonin-suppressing effect of traditional incandescent lighting
- Two hours of tablet reading can suppress melatonin by over 50%
- These effects can delay melatonin release by up to three hours
The ratio of blue to yellow light naturally changes at twilight, serving as a critical environmental cue for sleep timing. However, modern technology disrupts this pattern through:
- Increased exposure to short-wavelength blue light
- Sustained mental engagement from device use
- Disrupted circadian phase timing
- Reduced sleep period length
- Limited REM sleep occurrence is typically concentrated in the last part of sleep.

Evidence-Based Sleep Enhancement Strategies
Clinical research solidifies cognitive behavioural therapy for insomnia (CBT-I) as a transformative approach to sleep and restorative health enhancement. Meta-analyses reveal CBT-I participants achieve 85-90% improvement in sleep efficiency compared to 65% with medication.
CBT-I employs multiple evidence-backed components to restructure sleep patterns. Patients learn stimulus control techniques, strengthening the association between bed and sleep whilst breaking links with wakeful activities. Sleep restriction therapy temporarily reduces time in bed to build sleep pressure and consolidate fragmented sleep.
Advanced sleep monitoring through polysomnography (detailed overnight sleep study) identifies precise areas for intervention. Studies demonstrate that addressing sleep onset issues separately from sleep maintenance problems yields superior outcomes. Additionally, comprehensive assessment protocols examine medical conditions, psychological factors, and existing medications that might affect sleep quality.
Contemporary research highlights inflammatory mediators’ crucial role in sleep regulation. Clinical trials using specific inhibitors show remarkable success in reducing daytime fatigue. For instance, treatments targeting inflammatory proteins TNF and IL-1 significantly improve sleep quality in conditions like sleep apnoea.
Digital CBT-I programmes now extend treatment accessibility beyond traditional clinical settings. Systematic reviews confirm online interventions achieve comparable benefits to in-person therapy, with improvements in total sleep time and reduced wake periods. Furthermore, these digital platforms enable consistent monitoring of sleep patterns through integrated sleep diaries.
Extended sleep opportunity protocols demonstrate profound impacts on cognitive function. Young adults receiving 10-hour sleep opportunities over 14 consecutive nights showed marked improvements in alertness. Moreover, this extended sleep period enhanced memory consolidation and emotional regulation.
Treatment approaches increasingly emphasise personalised interventions based on specific sleep disruption patterns. Systematic assessment includes sleep history evaluation, symptom tracking, and screening for concurrent sleep disorders. Additionally, objective measurement through actigraphy (wrist-worn movement monitors) provides valuable data about sleep-wake patterns.
Managing Environmental and Lifestyle Factors for Better Sleep
Scientific evidence emphasises precise temperature control for optimal sleep and restorative health enhancement. Research identifies 18.3°C (65°F) as the ideal bedroom temperature, allowing proper core temperature reduction necessary for sleep initiation.
Temperature-sensitive neurons in the brain’s preoptic area actively regulate sleep onset. Local warming of this region promotes non-rapid eye movement sleep (NREM sleep, characterised by slower brain waves) and increases slow-wave activity. Subsequently, maintaining appropriate ambient temperature proves crucial for sustained sleep quality.
Nutritional timing significantly influences sleep architecture through immune system modulation. Research reveals complex interactions between dietary patterns and gut permeability, affecting sleep-regulatory substances. Furthermore, specific nutritional interventions demonstrate measurable improvements in sleep quality.
Physical activity timing requires careful consideration for sleep optimisation. Exercise influences core body temperature and immune system activation, affecting sleep-regulatory substances. Consequently, adequately timed physical activity enhances sleep quality without disrupting natural sleep onset.
Contemporary research identifies the social environment as a crucial sleep determinant. Communities with strong social cohesion report improved sleep duration and quality. Moreover, access to green spaces and natural water features correlates with reduced sleep insufficiency.
Mind-body practices show remarkable effectiveness in sleep improvement. Analysis of national health data reveals nearly 30% of individuals with sleep problems successfully utilise these approaches. Additionally, practices like tai chi and yoga demonstrate particular benefits for older adults.
Natural light exposure patterns significantly impact sleep regulation through melanopsin-containing retinal cells. These specialised photoreceptors respond specifically to blue light wavelengths, making them crucial for circadian rhythm regulation. Furthermore, prolonged exposure to bright natural light during waking hours correlates with enhanced sleep quality.

Optimising Sleep and Restorative Health Through Daily Habits
Molecular mechanisms controlling sleep and restorative health operate through sophisticated interactions between timing and pressure. Research demonstrates each cell contains daily cycles optimising energy acquisition, protection, repair, and reproduction.
Sleep architecture shows distinct mathematical patterns requiring consistent schedules for optimal function. Studies reveal how irregular sleep patterns disrupt standard sleep architecture and reduce efficiency. Moreover, recovery sleep following deprivation exhibits characteristic compensation patterns.
Advanced research illuminates the problematic relationship between sleep habits and immune function. Sleep regulatory substances, including immune system components, respond to neural activity patterns. Subsequently, excessive sensory stimulation enhances specific immune markers in cortical regions.
Experimental conditions with extended darkness windows yield significant benefits. Research participants exposed to 14-hour darkness periods, compared to typical 8-hour nights, demonstrated increased sleep duration. Furthermore, these individuals reported improved vigour and reduced fatigue levels.
Contemporary studies emphasise social engagement’s role in improving sleep quality. Regular social interaction combined with physical activity shows particular effectiveness for older adults. Additionally, morning or evening activity programmes demonstrate measurable improvements in neuropsychological performance.
Cardiac vagal tone (heart rate variability indicating parasympathetic nervous system activity) significantly correlates with sleep quality. Higher resting cardiac vagal tone is associated with reduced sleep latency and fewer disturbances. Furthermore, this physiological marker provides insight into autonomic nervous system balance during sleep.
Sleep and restorative health represent fundamental biological imperatives that profoundly influence physical well-being, cognitive function, and longevity. The intricate interplay between sleep architecture, environmental conditions, and consistent habits collectively determines sleep quality.
The body maintains crucial repair processes, immune function, and cognitive performance through optimal sleep patterns. The striking correlation between sleep quality and health outcomes reveals sleep as an essential pillar of human biology, vital for sustaining physical and mental vitality throughout life.
Sources
- Ackermann K, Revell VL, Lao O, Rombouts EJ, Skene DJ, Kayser M. Diurnal rhythms in blood cell populations and the effect of acute sleep deprivation in healthy young men. Sleep. 2012;35(7):933–40.
- Ahmadi S, Schütte S, Herlihy N. Health as a key driver of climate change communication. A scoping review. Preprints 2020:2020100095.
- Åkerstedt T., Schwarz J., Gruber G., Theorell-Haglöw J., Lindberg E. Short sleep-poor sleep? A polysomnographic study in a large population-based sample of women. J. Sleep Res. 2019;28:e12812.
- Aserinsky E, Kleitman N. Regularly occurring periods of eye motility and concomitant phenomena during sleep. Science 1953;118:273-4.
- Ballin M, Nordström P, Niklasson J, Nordström A. Associations of objectively measured physical activity and sedentary time with the risk of stroke, myocardial infarction or all-cause mortality. Sports Medicine 2021;51(2):339–349.
- Bassetti CL. Sleep and stroke. Semin Neurol. 2005 Mar;25(1):19-32.
- Baum KT, Desai A, Field J, Miller LE, Rausch J, Beebe DW. Sleep restriction worsens mood and emotion regulation in adolescents. J Child Psychol Psychiatry Allied Discip 2014;55:180–90.
- Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res 2003;12:1-12.
- Blake H, Gerard RW. Brain potentials during sleep. Am J Physiol 1937;119:692–703.
- Boyce R, Glasgow SD, Williams S, & Adamantidis A. Causal evidence for the role of REM sleep theta rhythm in contextual memory consolidation. Science, 352, 812–816.
- Brewster GS, Riegel B, Gehrman PR. Insomnia in the Older Adult. Sleep Med Clin. 2018 Mar;13(1):13-19.
- Cao J, Herman AB, West GB, Poe G, Savage VM. Unraveling why we sleep: Quantitative analysis reveals abrupt transition from neural reorganisation to repair in early development. vol. 6. 2020.
- Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta‐analysis of prospective studies. Eur Heart J. 2011;32:1482–
- Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis. SLEEP 2010;33(5):585-592.
- Chang A.M., Aeschbach D., Duffy J.F., Czeisler C.A. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc. Natl. Acad. Sci. USA. 2015;112:1232–1237.
- Dement W, Kleitman N. The relation of eye movements during sleep to dream activity: an objective method for the study of dreaming. J Exp Psychol 1957;53:339-46.
- Destexhe A, Sejnowski TJ. Interactions between membrane conductances underlying thalamocortical slow-wave oscillations. Physiol Rev 2003;83:1401-53.
- Diekelmann S, Born J. The memory function of sleep. Nat Rev Neurosci 2010;11:114–26.
- Everson CA. Sustained sleep-deprivation impairs host-defense. Am J Physiol. 1993;265(5):R1148–R54.
- Ferrara M., De Gennaro L., Bertini M. Selective slow-wave sleep (SWS) deprivation and SWS rebound: Do we need a fixed SWS amount per night? Sleep Res. Online. 1999;2:15–19.
- Ferguson T, Rowlands AV, Olds T, Maher C. The validity of consumer‐level, activity monitors in healthy adults worn in free‐living conditions: a cross‐sectional study. Int J Behav Nutr Phys Act. 2015;12:42.
- Folkard S, Åkerstedt T. Trends in the risk of accidents and injuries and their implications for models of fatigue and performance. Aviat Space Environ Med 2004;75:A161–7.
- Frank MG. Astroglial regulation of sleep homeostasis. Curr Opin Neurobiol 2013;23:812–18.
- Gao Y, Ge L, Liu M, Niu M, Chen Y, Sun Y, et al. Comparative efficacy and acceptability of cognitive behavioral therapy delivery formats for insomnia in adults: A systematic review and network meta-analysis. Sleep Med Rev. 2022 Aug;64:101648.
- Gradisar M, Wolfson AR, Harvey AG, et al. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med 2013;9(12):1291–9.
- Green A., Cohen-Zion M., Haim A., Dagan Y. Evening Light Exposure to Computer Screens Disrupts Human Sleep, Biological Rhythms, and Attention Abilities. Chronobiol. Int. 2017;34:855–865.
- Hammond EC. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am J Public Health Nations Health 1964;54:11–23.
- Hart N, Mandal S, Manuel A, et al. Obesity hypoventilation syndrome: does the current definition need revisiting? Thorax 2014;69:83–4.
- Haas HL, Sergeeva O, Selbach O. Histamine in the nervous system. Physiol Rev 2008;88:1183-241.
- Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place 2009;15(4):1006–13.
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, Hazen N, Herman J, Katz ES, Kheirandish-Gozal L, Neubauer DN, O’Donnell AE, Ohayon M, Peever J, Rawding R, Sachdeva RC, Setters B, Vitiello MV, Ware JC, Adams Hillard PJ. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015 Mar;1(1):40-43.
- Howorka K., Heger G., Schabmann A., Anderer P., Tribl G., Zeitlhofer J. Severe hypoglycaemia unawareness is associated with an early decrease in vigilance during hypoglycaemia. Psychoneuroendocrinology. 1996;21:295–312.
- Hubalek S, Brink M, Schierz C. Office workers’ daily exposure to light and its influence on sleep quality and mood. Lighting Res Technol. 2010;42:33-50.
- Irwin MR, Cole SW. Reciprocal regulation of the neural and innate immune systems. Nature Rev Immunol. 2011;11:625–32.
- Johnson DA, Simonelli G, Moore K. The neighborhood social environment and objective measures of sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2017;40(1).
- Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet 2014;383(9918):736–47.
- Kalsbeek, A., Buijs, R.M. Output pathways of the mammalian suprachiasmatic nucleus: coding circadian time by transmitter selection and specific targeting. Cell Tissue Res, 309 (2002), pp. 109-118.
- Knyazev GG. EEG delta oscillations as a correlate of basic homeostatic and motivational processes. Neurosci Biobehav Rev 2012;36:677–695.
- Koronowski K.B., Sassone-Corsi P. Communicating Clocks Shape Circadian Homeostasis. Science. 2021;371:eabd0951.
- Krauchi K. The thermophysiological cascasde leading to sleep initiation in relation to the phase of entrainment. Sleep Med Rev 2007;11:439-51.
- Krueger JM, Opp MR. Sleep and Microbes. Int Rev Neurobiol. 2016;131:207-225.
- Lamond N, Jay SM, Dorrian J, et al. The dynamics of neurobehavioural recovery following sleep loss. J Sleep Res 2007;16:33-41.
- Leary E.B., Watson K.T., Ancoli-Israel S., Redline S., Yaffe K., Ravelo L.A., Peppard P.E., Zou J., Goodman S.N., Mignot E., et al. Association of Rapid Eye Movement Sleep with Mortality in Middle-aged and Older Adults. JAMA Neurol. 2020;77:1241–1251.
- Lim AS, Yu L, Schneider JA, Bennett DA, Buchman AS. Sleep fragmentation, cerebral arteriolosclerosis, and brain infarct pathology in community‐dwelling older people. Stroke. 2016;47:516–518.
- Mehra R, Redline S. Sleep apnea: a proinflammatory disorder that coaggregates with obesity. J Allergy Clin Immunol 2008;121:1096–102.
- McCarley RW, Benoit O, Barrionuevo G. Lateral geniculate nucleus unitary discharge in sleep and waking: state-and rate-specific effects. J Neurophysiol 1983;50:798-818.
- McCusker RH, Kelley KW. Immune-neural connections: how the immune system’s response to infectious agents influences behavior. J Exp Biol 2013;216:84–98.
- McGinty D, Szymusiak R. Brain structures and mechanisms involved in the generation of NREM sleep: focus on the preoptic hypothalamus. Sleep Med Rev 2001;5:323-42.
- McGinty D, Szymusiak R. Hypothalamic regulation of sleep and arousal. Front Biosci 2003;8:1074-83.
- Middleton, B ∙ Stone, BM ∙ Arendt, J. Human circadian phase in 12:12 h, 200: <8 lux and 1000: <8 lux light-dark cycles, without scheduled sleep or activity. Neurosci Lett. 2002; 329:41-44.
- Mohammad-Zadeh L.F., Moses L., Gwaltney-Brant S.M. Serotonin: A Review. J. Vet. Pharmacol. Ther. 2008;31:187–199.
- Morin CM, Jarrin DC, Ivers H, Mérette C, LeBlanc M, Savard J. Incidence, Persistence, and Remission Rates of Insomnia Over 5 Years. JAMA Netw Open. 2020 Nov 02;3(11):e2018782.
- Naylor E, Penev PD, Orbeta L, Janssen I, Ortiz R, Colecchia EF, et al. Daily social and physical activity increases slow-wave sleep and daytime neuropsychological performance in the elderly. Sleep. 2000;23(1):87-95.
- Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111.
- Opp MR, Krueger JM. Sleep and immunity: a growing field with clinical impact. Brain Behav Immun 2015.
- Parrino L, Ferri R, Bruni O, Terzano MG. Cyclic alternating pattern (CAP): the marker of sleep instability. Sleep Med Rev 2012;16:27–45.
- Pase M.P., Himali J.J., Grima N.A., Beiser A.S., Satizabal C.L., Aparicio H.J., Thomas R.J., Gottlieb D.J., Auerbach S.H., Seshadri S. Sleep architecture and the risk of incident dementia in the community. Neurology. 2017;89:1244–1250.
- Pepin JL, Borel JC, Janssens JP, et al. Obesity hypoventilation syndrome: an under-diagnosed and undertreated condition. Am J Respir Crit Care Med 2012;186:1205–7.
- Riggins T. Longitudinal investigation of source memory reveals different developmental trajectories for item memory and binding. Dev Psychol 2014;50:449–59.
- Scammell, T.E. Narcolepsy. N. Engl. J. Med. 2015; 373:2654-2662.
- Siclari F, Baird B, Perogamvros L, Bernardi G, LaRocque JJ, Riedner B, Tononi G. The neural correlates of dreaming. Nature Neuroscience, 2017;20:872–878.
- Siegel JM. Clues to the functions of mammalian sleep. Nature, 437, 1264–1271.
- Smith MT, Perlis ML, Park A, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiatry. 2002;159(1):5-11.
- Song Y., Blackwell T., Yaffe K., Ancoli-Israel S., Redline S., Stone K.L. Relationships between sleep stages and changes in cognitive function in older men: The MrOS Sleep Study. Sleep. 2015;38:411–421.
- Spanò G, Gómez RL, Demara BI, Alt M, Cowen SL, Edgin JO. REM sleep in naps differentially relates to memory consolidation in typical preschoolers and children with Down syndrome. Proc Natl Acad Sci 2018;115:11844–9.
- Spiegel K, Tasali E, Penev P et al. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 141, 846–850.
- Tashiro M, Mochizuki H, Iwabuchi K, et al. Roles of histamine in regulation of arousal and cognition: Functional neuroimaging of histamine H1 receptors in human brain. Life Sci 2002;72:409-14.
- Van Cauter E, Plat L, Copinschi G. Interrelations between sleep and the somatotropic axis. Sleep 1998;21:533-66.
- Van Cauter E, Holmback U, Knutson K, et al. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007;67:2–9.
- VanHelder T., Symons J.D., Radomski M.W. Effects of Sleep Deprivation and Exercise on Glucose Tolerance. Aviat. Space Environ. Med. 1993;64:487–492.
- Vgontzas A, Bixler EO, Lin HM, et al. Chronic insomnia is associated with neurohumoral activation of the hypothalamo-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab 2001;86:3787-94.
- Voiß P, Höxtermann MD, Dobos G, Cramer H. The use of mind-body medicine among US individuals with sleep problems: analysis of the 2017 National Health Interview Survey data. Sleep Med. 2019;56:151-156.
- Wehr TA, Moul DE, Barbato G, Giesen HA, Seidel JA, Barker C, Bender C. Conservation of photoperiod-responsive mechanisms in humans. Am. J. Physiol. 1993;265:R846–R857.
- Werner GG, Ford BQ, Mauss IB, Schabus M, Blechert J, Wilhelm FH. High cardiac vagal control is related to better subjective and objective sleep quality. Biol Psychol. 2015;10679–85.
- Wesensten NJ, Belenky G, Thorne DR, et al. Modafinil vs. caffeine: effects on fatigue during sleep deprivation. Aviat Space Environ Med 2004;75:520–5.
- Zachariae R, Lyby MS, Ritterband LM, O’Toole MS. Efficacy of internet-delivered cognitive-behavioral therapy for insomnia – a systematic review and meta-analysis of randomised controlled trials. Sleep Med Rev. 2015;30:1-10.


