By BeSund Editorial Team 11/07/2023 Modified Date: 13/09/2024
Diabetes
Investigate the influence of regular exercise on diabetes
Diabetes and Fitness Management

Understanding Diabetes and Fitness Management
Diabetes and fitness management are closely linked, with physical activity playing a vital role in controlling this chronic metabolic disorder. Diabetes mellitus is characterised by elevated blood glucose levels resulting from defects in insulin secretion, action, or both. This condition affects millions worldwide, significantly impacting overall health and quality of life.
Diabetes can lead to severe complications, including cardiovascular disease, kidney failure, and nerve damage. Moreover, it increases the risk of blindness and lower limb amputations, underscoring the importance of effective management strategies.
Diabetes’s impact extends beyond individual health, placing a substantial burden on healthcare systems globally. Understanding this condition is crucial for developing comprehensive management approaches.
This wellness topic explores the fundamentals of diabetes, its global impact, and the vital connection between diabetes management and exercise.
Types of Diabetes and Their Characteristics
Understanding the types of diabetes is crucial for practical diabetes and fitness management. There are several types of diabetes, each with distinct characteristics and management needs. The two main types are Type 1 and Type 2 diabetes.
Type 1 Diabetes, previously known as juvenile diabetes, is an autoimmune condition in which the body’s immune system attacks insulin-producing cells in the pancreas. This type accounts for about 5-10% of all diabetes cases and typically develops in childhood or early adulthood.
Type 2 Diabetes is the most common form and accounts for 90-95% of all cases. It develops when the body becomes resistant to insulin or doesn’t produce enough insulin to maintain normal glucose levels.
The Global Burden of Diabetes: Trends and Statistics
The World Health Organization (WHO) mortality database provides crucial insights into the global impact of diabetes mellitus. This comprehensive resource offers a detailed account of medically-certified deaths worldwide, with a specific focus on diabetes. An interactive visualisation above reveals a stark increase in diabetes-related deaths from 1950 to 2022. In 1950, global deaths stood at approximately 7.6 million, with over 77,000 attributed to diabetes mellitus. By 2020, total deaths had risen to 31.7 million, while diabetes-related deaths had increased dramatically to 1.16 million – a fifteen-fold increase. This surge in diabetes mortality far outpaces the overall rise in deaths, which only quadrupled during the same period. Examining gender-specific trends reveals an essential shift in diabetes and fitness management. In 1950, female deaths from diabetes (48,062) significantly outnumbered male deaths (29,146). However, this pattern has reversed in recent decades. By 2020, male deaths from diabetes (587,842) slightly exceeded female deaths (569,210). This change highlights the evolving nature of diabetes risk factors and the need for gender-specific approaches in diabetes prevention and management. The more recent data for 2021 and 2022 show a drop in recorded deaths due to incomplete reporting, reflecting the nature of the WHO database, which updates figures gradually as more data becomes available. The WHO data further emphasises the urgency of addressing diabetes and fitness management globally. The number of people with diabetes rose from 108 million in 1980 to 422 million in 2014, with prevalence increasing more rapidly in low- and middle-income countries. Between 2000 and 2019, there was a 3% increase in age-standardised mortality rates from diabetes. In lower-middle-income countries, the mortality rate due to diabetes increased by 13%. These statistics highlight the critical need for practical diabetes and fitness management strategies to combat this growing global health challenge.
Diabetes and Fitness Management: A Crucial Connection
The relationship between diabetes and fitness management is fundamental to controlling this chronic condition. Regular physical activity is pivotal in managing blood glucose levels and enhancing overall health for individuals with diabetes. Exercise promotes glycaemic control by enhancing insulin action, thus improving blood glucose regulation. Moreover, physical activity contributes to weight management, cardiovascular health, and overall well-being, all crucial factors in diabetes care. Research indicates that regular physical activity may prevent or delay the onset of diabetes and its complications. Both aerobic and resistance exercises have shown benefits in improving insulin sensitivity and glucose control. The connection between diabetes and fitness management is critical in controlling this chronic condition. Regular physical activity is essential to diabetes care plans. It contributes to improved blood glucose regulation, weight management, and overall health.
The Impact of Diabetes on Physical Performance
Diabetes significantly influences an individual’s physical performance, affecting various exercise capacity and endurance aspects. Knowledge of these impacts is crucial for practical diabetes and fitness management, allowing individuals to optimise their physical activities and health outcomes.
Physiological Effects of Diabetes on Exercise Performance
Diabetes and fitness management strategies must consider the complex physiological effects of the condition on exercise performance. Several vital mechanisms contribute to altered physical capabilities and endurance in individuals with diabetes:
- Lipoprotein Lipase (LPL) Activity: Sedentary behaviour, often prevalent in individuals with diabetes, strongly influences LPL activity in skeletal muscles. LPL plays a crucial role in hydrolysing triglycerides in lipoproteins, and its alteration can significantly affect energy metabolism during exercise. This change in LPL activity can impact the body’s ability to utilise fats for energy, potentially affecting endurance and overall exercise performance.
- Insulin Resistance: Higher levels of circulating LPL have been linked to preferential use of lipids as an energy source, potentially leading to insulin resistance. This insulin resistance can impair glucose uptake during physical activity, affecting overall performance and endurance. Practical diabetes and fitness management must address this challenge to optimise exercise benefits.
- Gene Activation: Sedentary behaviour may influence diabetes development through its effect on gene activation and deactivation, potentially altering physiological responses to exercise. This genetic component adds another layer of complexity to diabetes and fitness management, emphasising the need for personalised approaches.
- Glycaemic Control: Poor glycaemic control can negatively affect exercise training adaptations, including maximal oxygen consumption, workload capacity, heart rate response, stroke volume, and cardiac output. These factors collectively impact an individual’s ability to perform and benefit from physical activities, highlighting the importance of maintaining stable blood glucose levels as part of diabetes and fitness management.
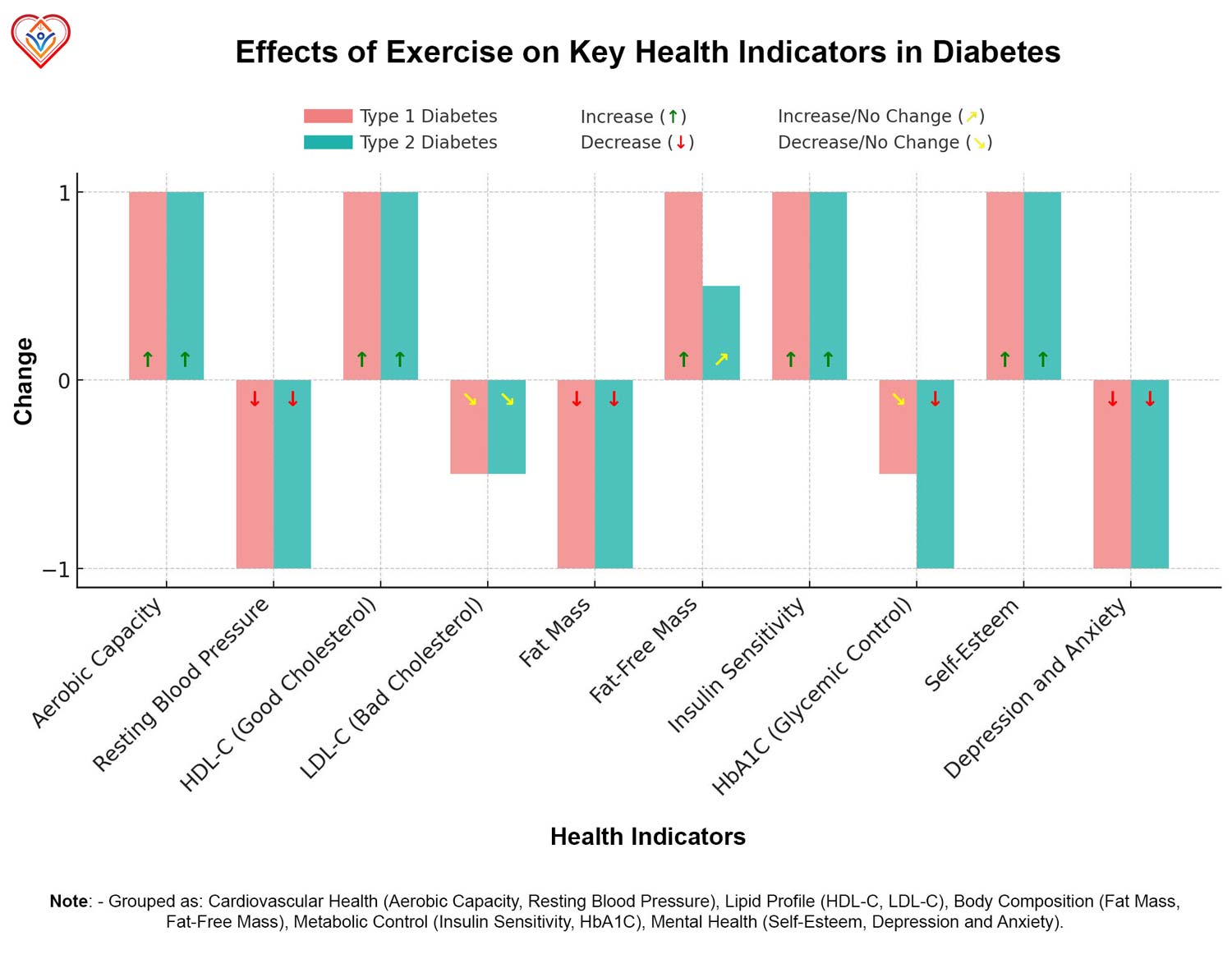
The effects of exercise on various health indicators for Type 1 and Type 2 diabetes are significant and multifaceted. As illustrated in the accompanying chart above, both types of diabetes show improvements in aerobic capacity and resting blood pressure with regular exercise. Additionally, the chart demonstrates positive changes in lipid profiles, particularly increases in HDL-C (good cholesterol) and decreases in LDL-C (bad cholesterol) for both types of diabetes. These improvements highlight the crucial role of exercise in diabetes and fitness management, reinforcing the need for tailored physical activity programmes. Blood sugar fluctuations can significantly affect exercise performance, presenting unique challenges in diabetes and fitness management:
- Hyperglycaemia: When blood glucose levels are poorly controlled, the liver’s glucose production increases, potentially resulting in higher blood glucose levels during exercise. This can lead to decreased exercise tolerance and performance.
- Hypoglycaemia: Conversely, moderate-intensity exercise can reduce blood glucose by increasing muscle flow and enhancing glucose absorption into cells. While beneficial for glucose control, this effect requires careful monitoring to prevent dangerously low blood sugar levels during or after exercise.
Challenges in Diabetes and Fitness Management During Physical Activities
Individuals with diabetes face several unique challenges during physical activities, necessitating careful consideration of diabetes and fitness management strategies. These challenges can significantly impact exercise performance, safety, and long-term health outcomes. One of the primary concerns is maintaining stable blood glucose levels during exercise. Rapid changes in glucose levels can lead to loss of control and fear of hypoglycaemia. This fear can be a significant barrier to regular physical activity, highlighting the need for education and support in diabetes and fitness management programmes. Moreover, the risk of nocturnal hypoglycaemia is elevated on nights following physical activity, requiring careful monitoring and management. This post-exercise effect emphasises the need for comprehensive diabetes and fitness management strategies beyond the actual exercise session. Thermoregulation presents another significant challenge, particularly for individuals with Type 2 diabetes. Research indicates an increased risk of heat stress during physical activity but not during passive rest. This is due to several factors:
- Impairments in whole-body heat loss
- Abnormal cutaneous vasodilation
- Decreased sweating capacity
These thermoregulatory issues can increase body temperature and heart rate during exercise, potentially limiting exercise capacity and increasing health risks. For individuals with Type 1 diabetes, insulin dosing becomes particularly challenging when exercise is involved. Exercise affects insulin sensitivity for many hours afterwards, making it challenging to balance insulin doses with physical activity and food intake. This complex interplay requires careful planning and monitoring as part of a comprehensive diabetes and fitness management approach. Another consideration is the depletion of glycogen stores during exercise. Limited muscle and liver glycogen are used during aerobic and resistance training, with effects on glycaemic levels often lasting several hours post-exercise. This prolonged effect necessitates strategies for replenishing energy stores and maintaining stable blood glucose levels in the hours following physical activity. Cardiovascular risks also pose a significant concern. Patients with diabetes are 2 to 4 times more likely than healthy individuals to suffer from cardiovascular disease, complicating exercise routines. This increased risk accentuates the need for careful cardiovascular assessment and monitoring as part of diabetes and fitness management programmes. Despite these challenges, regular physical activity remains crucial for managing diabetes. It can reduce the risk of developing impaired glucose tolerance, insulin resistance, and type 2 diabetes. Moreover, maintaining cardiovascular fitness is a strong predictor of all-cause mortality in patients with type 2 diabetes. Exercise intensity plays a vital role in managing diabetes, with research indicating that higher-intensity exercise may offer additional benefits. More significant reductions in HbA1c (overall glycaemic control), a key indicator of long-term blood glucose control, have been observed with more intense exercise. However, the intensity and type of training must be carefully balanced with individual capabilities and health status. Given individuals’ unique challenges with diabetes, personalised exercise programmes that consider these factors are essential for practical diabetes and fitness management. These programmes should address not only the physical aspects of exercise but also the psychological barriers and long-term health implications associated with diabetes. 
Exercise as a Management Tool for Diabetes
Exercise plays a pivotal role in diabetes and fitness management, offering numerous benefits for individuals with Type 1 and Type 2 diabetes. Regular physical activity can significantly improve glycaemic control, enhance insulin sensitivity, and reduce the risk of diabetes-related complications. Types of exercises beneficial for diabetes management:
- Aerobic exercise: Brisk walking, cycling, or swimming can improve cardiovascular health and help control blood glucose levels.
- Resistance training: Strength exercises using weights or resistance bands can enhance muscle mass and improve insulin sensitivity.
- High-intensity interval training (HIIT): Short bursts of intense activity followed by rest periods can provide significant benefits in a time-efficient manner.
- Combined training: A mix of aerobic and resistance exercises may offer more significant benefits than either type alone.
Regular physical activity is crucial for diabetes and fitness management, as it helps improve insulin sensitivity. This improvement occurs through several mechanisms:
- Enhanced glucose uptake: Exercise increases the body’s ability to transport glucose from the bloodstream into muscle cells, even without insulin.
- Increased muscle mass: Resistance training, in particular, can build muscle tissue, which is more responsive to insulin and can help lower blood glucose levels.
- Improved mitochondrial function: Regular exercise enhances the efficiency of cellular energy production, contributing to better glucose metabolism.
Evidence showing exercise’s impact on long-term diabetes control is substantial. Studies have demonstrated that consistent physical activity can lead to:
- Reduced HbA1c levels: Regular exercise can lower glycated haemoglobin levels by 0.5-0.7%, indicating improved long-term blood glucose control.
- Decreased medication requirements: Some individuals may be able to reduce their diabetes medication or insulin doses with a consistent exercise program.
- Improved cardiovascular health: Exercise can help manage blood pressure and cholesterol levels, reducing the risk of heart disease associated with diabetes.
Potential benefits of exercise for diabetes and fitness management extend beyond glycaemic control:
- Weight management: Regular physical activity can help individuals maintain a healthy weight or lose excess body fat, particularly beneficial for those with Type 2 diabetes.
- Enhanced mental well-being: Exercise has been shown to improve mood, reduce stress, and enhance overall quality of life for individuals with diabetes.
- Reduced risk of complications: Consistent physical activity can lower the risk of diabetes-related complications such as neuropathy and cardiovascular disease.
- Improved sleep quality: Regular exercise can enhance sleep patterns, essential for overall health and glucose regulation.
It’s important to note that the benefits of exercise in diabetes and fitness management are dose-dependent. Current guidelines recommend at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, along with resistance training at least twice a week. While exercise is a powerful tool for diabetes management, individuals must work with their healthcare providers to develop a safe and effective exercise programme. This approach ensures that the exercise program is tailored to the individual’s needs, considering factors such as current fitness level, diabetes type, and any existing complications.
Recommended Exercises for Diabetes and Fitness Management
Exercise plays a crucial role in diabetes and fitness management, offering numerous benefits for individuals with Type 1 and Type 2 diabetes. A well-structured exercise programme can help control blood glucose levels, improve insulin sensitivity, and reduce the risk of diabetes-related complications. When developing an exercise plan for diabetes management, it’s essential to consider the individual’s current fitness level, any existing complications, and personal preferences. A comprehensive approach should include a combination of aerobic exercises, strength training, and flexibility work to maximise the benefits of physical activity. Aerobic exercises are particularly beneficial for individuals with diabetes as they help improve cardiovascular health and enhance glucose metabolism. Brisk walking, cycling, swimming, and dance-based exercises can effectively manage blood glucose levels and improve overall fitness. Low-impact options like water aerobics or stationary cycling may be more suitable for those with limited mobility or joint issues. Strength training is another essential component of a diabetes-focused exercise programme. Resistance exercises help build lean muscle mass, which can improve insulin sensitivity and glucose uptake. Resistance bands, weight machines, or bodyweight exercises can effectively develop strength and manage diabetes. Starting with lighter weights and gradually increasing intensity is essential to avoid injury and ensure proper form. Flexibility and balance exercises contribute to overall fitness. They can be particularly beneficial for individuals with diabetes who may be at risk of joint stiffness or balance issues. Stretching routines, yoga, and tai chi can improve flexibility, reduce the risk of injury, and enhance overall well-being. These exercises can also help manage stress, an important factor in diabetes management.
Types of Exercises for Diabetes Management
Various exercise types can benefit individuals with diabetes, offering unique advantages for managing blood glucose levels and improving overall fitness. The following categories of exercises are particularly effective for diabetes and fitness management
- Aerobic Exercises:
- Brisk walking
- Cycling (outdoor or stationary)
- Swimming or water aerobics
- Dancing
- Low-impact aerobics classes
- Strength Training:
- Resistance band exercises
- Body weight exercises (e.g., squats, push-ups, lunges)
- Weight machine exercises
- Dumbbell or kettlebell workouts
- Flexibility and Balance:
- Stretching routines
- Yoga
- Tai chi
- Pilates
- Combination Workouts:
- Circuit training (combining aerobic and strength exercises)
- Interval training (alternating between high and low-intensity periods)
When adapting exercises for different stages or severities of diabetes, it’s crucial to consider any existing complications or limitations. For individuals with neuropathy, low-impact exercises and proper footwear are essential to prevent foot injuries. Those with retinopathy should avoid exercises that dramatically increase blood pressure, such as weightlifting. Always consult with a healthcare professional before starting a new exercise programme, especially if you have existing diabetes-related complications.
FITT Recommendations for Individuals with Diabetes
The FITT principle (Frequency, Intensity, Time, and Type) provides a framework for structuring exercise programmes for individuals with diabetes. Here are the FITT recommendations based on current guidelines: Aerobic Exercise:
- Frequency:
- Type 1 Diabetes: 3-7 days per week
- Type 2 Diabetes: 3-7 days per week, with no more than two consecutive days without exercise
- Intensity:
- Type 1 and Type 2 Diabetes: Moderate (40%-59% of VO₂ reserve or 11-12 on the Rating of Perceived Exertion [RPE] scale) to vigorous (60%-89% of VO₂ reserve or 14-17 on the RPE scale)
- Time:
- Type 1 Diabetes: At least 150 minutes per week of moderate-intensity or 75 minutes of vigorous-intensity exercise
- Type 2 Diabetes: Minimum 150 minutes per week of moderate-to-vigorous intensity exercise
- Type:
- Type 1 and Type 2 Diabetes: Large muscle group activities such as walking, cycling, swimming, or dancing
Resistance Exercise:
- Frequency:
- Type 1 and Type 2 Diabetes: 2-3 non-consecutive days per week
- Intensity:
- Type 1 and Type 2 Diabetes: Moderate (50%-69% of 1-repetition maximum) to vigorous (70%-85% of 1-repetition maximum)
- Time:
- Type 1 and Type 2 Diabetes: 8-10 exercises with 1-3 sets of 10-15 repetitions to near fatigue per set
- Type:
- Type 1 and Type 2 Diabetes: Resistance machines, free weights, bodyweight exercises, or resistance bands
Flexibility Exercise:
- Frequency:
- Type 1 and Type 2 Diabetes: 2-3 days per week, ideally daily
- Intensity:
- Type 1 and Type 2 Diabetes: Stretch to the point of tightness or slight discomfort, not pain
- Time:
- Type 1 and Type 2 Diabetes: 10-30 seconds per stretch, 2-4 repetitions for each stretch
- Type:
- Type 1 and Type 2 Diabetes: Static or dynamic stretching, yoga, or tai chi
These FITT recommendations provide a general guideline for diabetes and fitness management. However, it’s essential to tailor these recommendations to individual needs, fitness levels, and any existing complications.
Safety Measures and Precautions for Exercising with Diabetes
Exercising with diabetes requires careful planning and monitoring to ensure safety and optimal benefits. Diabetes and fitness management strategies should include specific safety measures tailored to individual needs. Those with diabetes can enjoy the numerous advantages of regular physical activity. Important Safety Tips:
- Carry identification: Always wear a medical ID bracelet or carry a card stating you have diabetes.
- Stay hydrated: Drink water before, during, and after exercise to prevent dehydration.
- Wear appropriate footwear: Choose comfortable, well-fitting shoes to protect your feet from injury.
- Warm-up and cool down: Gradually increase and decrease exercise intensity to avoid sudden blood sugar changes.
- Exercise with a partner: When possible, work out with someone who knows about your condition.
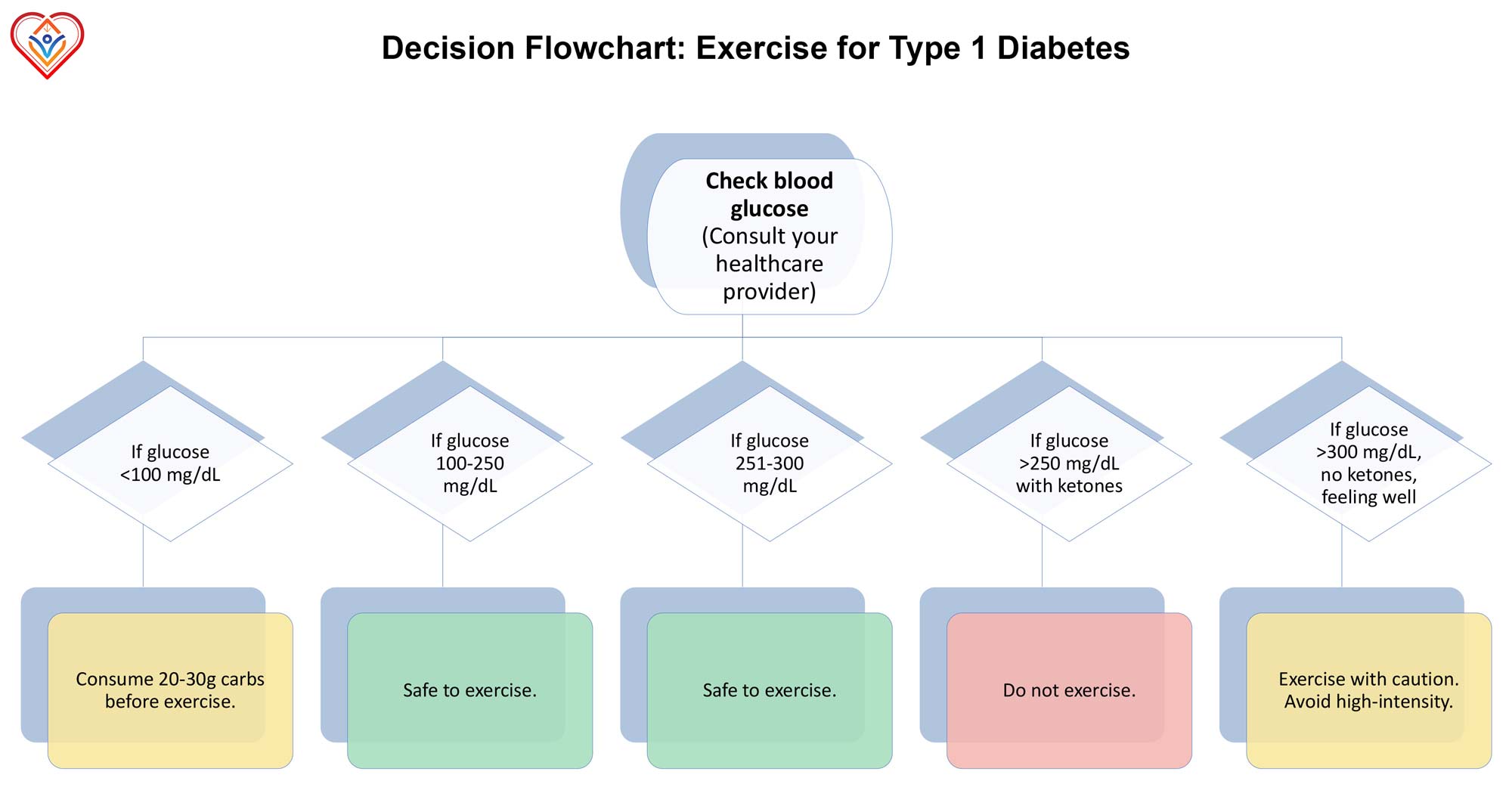
Blood Sugar Monitoring: Regularly checking blood glucose levels is crucial for diabetes and fitness management during exercise. The chart above provides a helpful guide for making exercise decisions based on blood glucose readings. Consider the following monitoring practices:
- Before exercise: Check your blood sugar 15-30 minutes before starting your workout.
- During exercise: For longer sessions, monitor your levels every 30 minutes.
- After exercise: Check your blood sugar immediately after and several hours post-workout.
Adjusting Medication and Insulin: Physical activity can significantly impact blood glucose levels, necessitating adjustments to medication or insulin dosages. Consider these guidelines:
- Reduce insulin doses before planned exercise to prevent hypoglycaemia.
- For spontaneous activities, consume additional carbohydrates to balance glucose levels.
- Keep fast-acting carbohydrates on hand during workouts in case of sudden drops in blood sugar.
Consulting Healthcare Providers: Regular communication with your healthcare team is essential for safe diabetes and fitness management. Seek professional advice in the following situations:
- Before starting a new exercise program
- If experiencing frequent hypoglycaemia during or after workouts
- When adjusting medication or insulin doses for physical activity
- If you develop any diabetes-related complications
By integrating these safety measures and precautions into your exercise routine, you can effectively manage diabetes while reaping the benefits of physical activity. Listen to your body and adjust your approach for optimal health outcomes. 
Diabetes and Fitness Management: Lifestyle Tips for Daily Living
Practical diabetes and fitness management extend beyond exercise routines and medical interventions. It encompasses a holistic approach to daily living, incorporating mindful habits and lifestyle modifications. Cultivating supportive daily habits is crucial for successful diabetes and fitness management. Regular sleep patterns are vital in maintaining stable blood glucose levels and improving insulin sensitivity. Aim for 7-9 hours of quality sleep each night to support your body’s natural rhythms and metabolic processes. Nutritional choices significantly impact blood sugar control and complement physical activity in diabetes and fitness management. A balanced diet of whole grains, lean proteins, and healthy fats can help stabilise blood glucose levels. Incorporating fibre-rich foods, such as vegetables, fruits, and legumes, can slow down glucose absorption and improve overall glycaemic control. Mindful eating practices, such as portion control and regular meal timing, contribute to better diabetes management. Consider using the plate method, where half your plate consists of non-starchy vegetables, a quarter contains lean protein, and the remainder includes whole grains or starchy vegetables. Stress management is an often-overlooked aspect of diabetes and fitness management. Chronic stress can lead to elevated blood glucose levels and hinder overall health. Incorporating relaxation techniques like deep breathing exercises, meditation, or yoga can help mitigate stress-induced glucose fluctuations. Engaging in hobbies or activities that bring joy and relaxation can also reduce stress. Whether gardening, reading, or practising a musical instrument, finding moments of calm in daily life supports overall well-being and diabetes management. Long-term strategies for diabetes and fitness management involve creating sustainable lifestyle modifications. Regular health check-ups and ongoing education about diabetes management are essential. Stay informed about the latest developments in diabetes care and be proactive in discussing new treatment options with your healthcare team. Building a support network is invaluable for long-term diabetes and fitness management. Connecting with others with diabetes through support groups or online communities can provide emotional support, practical tips, and motivation to maintain healthy habits. Embracing technology can enhance diabetes management efforts. Utilising smartphone apps for tracking blood glucose levels, physical activity, and nutrition can provide valuable insights and help identify patterns in your health data. Diabetes and fitness management are inextricably linked, with physical activity crucial in controlling blood glucose levels and improving overall health outcomes. Throughout this post, we’ve explored various aspects of exercise and its impact on diabetes management. From aerobic activities to strength training, the benefits of a well-rounded fitness routine are straightforward for individuals with Type 1 and Type 2 diabetes. Regular exercise helps manage blood glucose levels, enhances insulin sensitivity, reduces cardiovascular risk factors, and contributes to weight management. The FITT recommendations offer a structured approach to incorporating fitness into daily life. The safety measures discussed ensure that individuals can exercise effectively and safely. Combining these fitness strategies with the lifestyle tips outlined, individuals with diabetes can create a comprehensive approach to managing their condition and improving their overall quality of life.
Sources
- American Diabetes Association (2021). Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2021. Diabetes Care, 44(Supplement 1), S53-S72.
- American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care. 2016;39(suppl 1):S13–22.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1):S62–9.
- Baldi, J. C., Cassuto, N. A., Foxx-Lupo, W. T., Wheatley, C. M., & Snyder, E. M. (2010). Glycemic status affects cardiopulmonary exercise response in athletes with type I diabetes. Medicine and Science in Sports and Exercise, 42(8), 1454-1459.
- Bey, L., & Hamilton, M. T. (2003). Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. The Journal of Physiology, 551(2), 673-682.
- Bey, L., Akunuri, N., Zhao, P., Hoffman, E. P., Hamilton, D. G., & Hamilton, M. T. (2003). Global gene expression patterns in rat skeletal muscle during unloading and low-intensity ambulatory activity. Physiological Genomics, 13(2), 157-167.
- Boulé, N. G., Kenny, G. P., Haddad, E., Wells, G. A., & Sigal, R. J. (2003). Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in Type 2 diabetes mellitus. Diabetologia, 46(8), 1071-1081.
- Boulé NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. 2001;286(10):1218–27.
- Centres for Disease Control and Prevention. National Diabetes Statistics Report, 2024 [Internet]. Atlanta (GA): US Department of Health and Human Services.
- Chimen, M., Kennedy, A., Nirantharakumar, K., Pang, T. T., Andrews, R., & Narendran, P. (2012). What are the health benefits of physical activity in type 1 diabetes mellitus? A literature review. Diabetologia, 55(3), 542-551.
- Chudyk A, Petrella RJ. Effects of exercise on cardiovascular risk factors in type 2 diabetes: a meta-analysis. Diabetes Care. 2011;34(5):1228–37.
- Church TS, Blair SN, Cocreham S, et al. Effects of aerobic and resistance training on haemoglobin A1c levels in patients with type 2 diabetes: a randomised controlled trial. JAMA. 2010;304:2253–62.
- Colberg SR, Albright AL, Blissmer BJ, et al. Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: a joint position statement. Exercise and type 2 diabetes. Med Sci Sports Exerc. 2010;42(12):2282–303.
- Colberg SR, Sigal RJ, Yardley JE, et al. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016;39:2065–79.
- Delvecchio, M., Zecchino, C., Salzano, G., Faienza, M. F., Cavallo, L., De Luca, F., & Lombardo, F. (2009). Effects of moderate-severe exercise on blood glucose in Type 1 diabetic adolescents treated with insulin pump or glargine insulin. Journal of Endocrinological Investigation, 32(6), 519-524.
- Dunstan, D.W., Daly, R.M., Owen, N., Jolley, D., De Courten, M., Shaw, J., and Zimmet, P. (2002). High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care, 25(10), 1729-1736.
- Egan, B., & Zierath, J. R. (2013). Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metabolism, 17(2), 162-184.
- Ferreira, L. D., Pulawa, L. K., Jensen, D. R., & Eckel, R. H. (2001). Overexpressing human lipoprotein lipase in mouse skeletal muscle is associated with insulin resistance. Diabetes, 50(5), 1064-1068.
- Haffner, S. M., Lehto, S., Rönnemaa, T., Pyörälä, K., & Laakso, M. (1998). Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. New England Journal of Medicine, 339(4), 229-234.
- Herriott, M.T., Colberg, S.R., Parson, H.K., Nunnold, T., and Vinik, AI (2004). Effects of 8 weeks of flexibility and resistance training in older adults with type 2 diabetes. Diabetes Care, 27(12), 2988-2989.
- Huai P, Han H, Reilly KH, Guo X, Zhang J, Xu A. Leisure-time physical activity and risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Endocrine. 2016;52(2):226–30.
- Kosuri, M., & Sridhar, G. R. (2018). Yoga practice in diabetes improves physical and psychological outcomes. Metabolic syndrome and related disorders, 16(1), 33-39.
- Litchman, M. L., Walker, H. R., Ng, A. H., Wawrzynski, S. E., Oser, S. M., Greenwood, D. A., … & Oser, T. K. (2019). State of the science: A scoping review and gap analysis of diabetes online communities. Journal of diabetes science and technology, 13(3), 466-492.
- Ostman, C., Jewiss, D., King, N., & Smart, N. A. (2018). Clinical outcomes to exercise training in type 1 diabetes: A systematic review and meta-analysis. Diabetes Research and Clinical Practice, 139, 380-391.
- Phielix E, Meex R, Moonen-Kornips E, Hesselink MK, Schrauwen P. Exercise training increases mitochondrial content and ex vivo mitochondrial function similarly in patients with type 2 diabetes and in control individuals. Diabetologia. 2010;53(8):1714–21.
- Poirier, M. P., Notley, S. R., Boulay, P., Sigal, R. J., Friesen, B. J., Malcolm, J., … & Kenny, G. P. (2020). Type 2 diabetes does not exacerbate body heat storage in older adults during brief, extreme passive heat exposure. Temperature, 7(3), 263-269.
- Reddy, R., El Youssef, J., Winters-Stone, K., Branigan, D., Leitschuh, J., Castle, J., & Jacobs, P. G. (2018). The effect of exercise on sleep in adults with type 1 diabetes. Diabetes, Obesity and Metabolism, 20(2), 443-447.
- Reutrakul, S., & Van Cauter, E. (2018). Sleep influences obesity, insulin resistance, and risk of type 2 diabetes. Metabolism, 84, 56-66.
- Reynolds, A. N., Mann, J. I., Cummings, J., Winter, N., Mete, E., & Te Morenga, L. (2020). Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet, 393(10170), 434-445
- Riddell, M.C., Gallen, I.W., Smart, C.E., Taplin, C.E., Adolfsson, P., Lumb, A.N., Kowalski, A., Rabasa-Lhoret, R., McCrimmon, R.J., Hume, C., Annan, F., Fournier, P.A., Graham, C., Bode, B., Galassetti, P., Jones, T.W., Millán, I.S., Heise, T., Peters, A.L., Petz, A., and Laffel, L.M. (2017). Exercise management in type 1 diabetes: a consensus statement. The Lancet Diabetes & Endocrinology, 5(5), 377-390.
- Tarp, J., Støle, A.P., Blond, K., and Grøntved, A. (2019). Cardiorespiratory fitness, muscular strength and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetologia, 62(7), 1129-1142.
- Wei, M., Gibbons, L. W., Kampert, J. B., Nichaman, M. Z., & Blair, S. N. (2000). Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Annals of Internal Medicine, 132(8), 605-611.
- Williamson DA, Rejeski J, Lang W, Van Dorsten B, Fabricatore AN, Toledo K, Look ARG. Impact of a weight management program on health-related quality of life in overweight adults with type 2 diabetes. Arch Intern Med. 2009;169:163-171.
- World Health Organization. The WHO mortality database for Diabetes mellitus.
- World Health Organization. 5 April 2023. ‘Diabetes‘.
- Yardley, J. E., & Sigal, R. J. (2015). Exercise strategies for hypoglycemia prevention in individuals with type 1 diabetes. Diabetes Spectrum, 28(1), 32-38.
- Zanuso, S., Jimenez, A., Pugliese, G., Corigliano, G., & Balducci, S. (2010). Exercise for managing type 2 diabetes: a review of the evidence. Acta Diabetologica, 47(1), 15-22.


