By BeSund Editorial Team 11/07/2023 Modified Date: 03/05/2024
Arthritis and Joint Health
Learn about the impact of exercise on joint health and arthritis
Arthritis and Joint Health for Active Living

Understanding Arthritis and Joint Health for Active Living
Arthritis and joint health for active living is a subject that influences the daily lives of millions globally. Arthritis, a chronic ailment, is the cause of impaired function in adults and manifests in over 100 different forms.
Different Forms of Arthritis and Joint Health for Active Living
These forms can be broadly categorised into osteoarthritis (OA), rheumatoid arthritis (RA), fibromyalgia, and spondyloarthropathies (SA). Each state has its unique characteristics. For instance, OA is mainly confined to specific joints and often occurs due to age, trauma, or infection. On the other hand, RA and other systemic forms affect multiple tissues and can be more debilitating.
Symptoms Common to Arthritis
Symptoms such as stiffness, joint or muscle pain, and fatigue are commonly observed across all forms of arthritis. However, it’s worth noting that exercise, contrary to popular belief, can effectively manage these symptoms. Properly guided physical activity can reduce pain and help maintain regular joint function. Several risk factors can make an individual more susceptible to arthritis. These include advancing age, being female, and lifestyle elements such as being overweight, sustaining joint injuries, or having occupations that strain the joints. Smoking has also been identified as a risk factor specifically for RA. The diagnostic process for arthritis usually involves a combination of health history, physical examination, X-ray imaging, and laboratory tests. A peculiar observation is that morning stiffness can act as an indicator of the type of arthritis. If the stiffness lasts less than 30 minutes, it’s often OA; it lasts longer for systemic forms. The benefits of increased physical activity for arthritis management have been substantiated through multiple studies. However, incorporating physical activity improvement methods in routine clinical care for arthritis patients remains challenging.
Arthritis and Joint Health for Active Living: What We Will Cover
In the following sections, we’ll explore how arthritis and joint health for active living affect physical performance. We will discuss exercise as a potent management tool, recommend arthritis-friendly exercises, and offer safety guidelines and lifestyle tips for an active life with Arthritis and Joint Health. 
The Impact of Arthritis and Joint Health on Physical Performance
Arthritis and joint health for active living are fundamental aspects that profoundly hamper physical performance, making even simple tasks strenuous. The condition deteriorates cartilage, causing increased friction and joint pain during activities like walking or standing. This is particularly evident in osteoarthritis of the knee. Where the absence of protective cartilage leads to dynamic knee loads that cause pain and significantly affect gait patterns in both males and females.
How Arthritis Affects Physical Tasks for Active Living
The impact of arthritis and joint health on active living isn’t confined to the elderly only. It affects physical performance across various age groups. Gender-specific considerations also come into play. Studies indicate that females may experience different gait biomechanics than males when afflicted with osteoarthritis. This divergence between genders suggests that treatment interventions should be tailored to address these differences to effectively manage the condition. Arthritis and joint health for active living take a significant toll, not just on physical capabilities but also on overall well-being. One of the most telling indicators is the array of characteristic signs and symptoms of rheumatoid arthritis. These signs and symptoms are multifaceted and systemic, profoundly affecting individuals’ quality of life. To get a better understanding, let’s consider some of these characteristic signs and symptoms:
- Pain, Swelling, Inflammation, and Tenderness: These symptoms often affect multiple joints, termed as polyarticular. They primarily occur bilaterally, impacting both sides of the body.
- Small Joints Affected First: Initially, the wrist and hand joints are the primary targets, serving as early indicators of the disease.
- Joint Deformities: Subluxation, ulnar drift, and swan-neck deformities are common and can severely limit mobility.
- Firm, Painless Growths: RA nodules can appear under the skin near the joints.
- Stiffness in Joints: This is particularly noticeable after rest and during morning hours.
- General Feeling of Fatigue: This can be overwhelming and is often accompanied by a decline in physical activity.
- Sleep Disturbances: Difficulty in maintaining a restful sleep is common among those affected by arthritis.
- Fear of Physical Activity and Depression: These psychological symptoms often co-occur, impacting the individual’s mental well-being.
- Radiographic Evidence: X-ray images often show joint erosion and destruction.
- Laboratory Values: Tests often show positive results for rheumatoid factor.
- Anti-citrullinated Protein Antibody: Also often found positive in lab tests.
- Abnormal C-Reactive Protein: This is usually elevated during acute phases of the disease.
- Elevated Erythrocyte Sedimentation Rate: Another typical lab finding indicative of inflammation.
Detailed Symptoms of Rheumatoid Arthritis
Understanding how arthritis affects joint health is crucial for active living. Below, we will explore the biomechanical and neurological factors that impact physical performance in individuals with osteoarthritis and rheumatoid arthritis. For those focused on arthritis and joint health for active living, grasping these changes can guide more effective management strategies. 1. Biomechanical Differences in Gait Patients with osteoarthritis display unique gait patterns compared to healthy individuals. Notable changes include increased knee adduction and decreased knee flexion. Gender-specific differences also exist; osteoarthritic females exhibit distinct gait biomechanics not observed in males. 2. Proprioception and Postural Sway A less obvious but significant factor is the loss of proprioception, the sense of body position, often overlooked in individuals with knee osteoarthritis. This can increase postural sway and expedite the arthritic process through ‘neurogenic acceleration’. 3. Muscle Activation and Strength Quadriceps weakness has been identified as a causative factor for knee osteoarthritis. It’s not just muscle weakness; the muscle’s inability to contract efficiently is also a concern. 4. Hip Osteoarthritis and Load Bearing Hip osteoarthritis poses another challenge, mainly as the hip is a critical load-bearing joint. Arthritic joints often display autogenous muscle inhibition, where surrounding muscles become weak and inhibited. 5. Intervention Strategies Elastic knee bandages can improve proprioception by 40%, suggesting that external supports offer valuable proprioceptive feedback. 6. Rheumatoid Arthritis In the case of rheumatoid arthritis, symptoms like joint deformities and firm, painless growths under the skin near joints are common. RA also affects sleep and psychological well-being, increasing fear of physical activity and contributing to depression. 
Exercise as a Management Tool for Arthritis and Joint Health
Exercise offers a multifaceted approach to managing Rheumatoid Arthritis (RA). It ameliorates pain and fatigue and elevates functional ability and cardiorespiratory fitness. This contributes positively to arthritis and joint health for active living. Significantly, exercise doesn’t exacerbate RA symptoms; it’s a safe practice that minimises healthcare costs through fewer hospital admissions. Osteoarthritis (OA) patients also gain substantially from regular exercise, a cornerstone in OA management protocols. Exercise aids joint mobility and fortifies the muscles around the affected joints, alleviating pain and enhancing overall physical function. Walking and strength training, in particular, have been shown to significantly reduce pain and disability in hip or knee OA patients, further supporting arthritis and joint health for active living. Water-based activities like swimming offer a dual benefit for both OA and RA sufferers. Aquatic exercise improves symptoms and augments the quality of life by providing resistance without putting stress on the joints. This makes it an ideal choice for joint pain or mobility issues. Aligning well with promoting arthritis and joint health for active living. Tai chi is another potent tool in the arsenal against OA, specifically for knee-related issues. This mind-body exercise entails slow, coordinated movements, effectively reducing pain and improving function. However, the advantages of exercise extend beyond joint health. Physical activity has been shown to mitigate systemic symptoms in RA, such as cardiovascular health, thereby contributing to a more comprehensive treatment strategy. When planning an exercise regimen for RA, several considerations should be made. The program must be individualised, considering the patient’s physical health and comorbid conditions like osteoporosis or atherosclerosis. Exercise activities causing pain should be modified or replaced, and any worsening of symptoms should lead to immediate termination of the exercise and consultation with healthcare providers. It’s crucial to start at low intensities and gradually ramp up, constantly monitoring symptoms to ensure safety and efficacy. These tailored programs aim to improve function while avoiding detrimental effects like joint pain, inflammation, and instability, thus facilitating a lifestyle change incorporating exercise and promoting arthritis and joint health for active living. 
Recommended Exercises for Individuals with Arthritis and Joint Health for Active Living
Arthritis and joint health for active living are contrasting terms. Still, they can co-exist through an evidence-based approach to exercise. Studies have shown that osteoarthritis sufferers who engage in a carefully selected range of physical activities can experience less joint pain and improve function. Exercise combats the stiffness commonly associated with arthritis, contributing to bone health, muscle strengthening, and improved balance. The science is precise: exercise can be a powerful tool in managing arthritis symptoms, even for active people. For many, “arthritis” conjures images of a life constrained by joint pain and limited mobility. However, the landscape is changing with emerging research that supports exercise’s role in managing arthritis symptoms. Exercise programmes must, however, be tailored to individual capabilities. It should be focused on improving joint flexibility, building muscle strength, and reducing inflammation. A meta-analysis of 54 clinical trials found that moderate physical activity could ease the pain experienced by arthritis patients by up to 40%. While research strongly supports exercise to manage arthritis, it’s crucial to note that not all exercises suit everyone. The focus should be on activities that can be realistically sustained and will maximise the benefits while minimising the risk of flare-ups. The following list offers evidence-based exercise recommendations that align with general guidelines for those dealing with arthritis and joint health issues.
- Land-based Aerobic Training: For those focusing on arthritis and joint health for active living, land-based aerobic training shows moderate effects on aerobic capacity, pain, and quality of life in individuals with rheumatoid arthritis.
- Combined Aerobic and Resistance Training: Combined training positively influences aerobic capacity and cardiovascular disease risk factors such as body composition and systemic inflammation.
- Resistance Training: Resistance training increases muscle performance in the upper and lower extremities, including grip strength.
- Walking: Walking serves as a functional aerobic activity, particularly for those who used to be runners.
- Cycling: Cycling is another effective aerobic activity that significantly benefits individuals with arthritis.
- Aquatic Exercise: Aquatic exercises can improve pain, strength, and overall function, especially for those with rheumatoid arthritis.
- Tai Chi: Tai Chi improves lower extremity strength, flexibility, and some aerobic benefits.
- Yoga: Yoga can notably improve function and balance, offering a complementary approach to arthritis and joint health for active living.
- Wall-Sit: Wall-sits strengthen the quadriceps while reducing knee pressure, which is particularly beneficial for knee arthritis.
- Resistance Bands: Resistance bands provide a scalable approach to strengthening exercises in the upper and lower extremities.
- Neuromuscular Training: Balance, agility, and proprioception exercises, done 2-3 times per week, can be highly effective.
- Static Stretching: Static stretches, held for 10-30 seconds, are recommended for improving flexibility.
Exercise Types and Their Specific Benefits for Arthritis and Joint Health
A frequently asked question regarding arthritis and joint health for active living is whether running exacerbates arthritis. While running exerts more pressure on joints than walking, no scientific evidence suggests it causes arthritis. Surprisingly, moderate running can alleviate some arthritis symptoms and improve function compared to a sedentary lifestyle. Now, let’s explore some specific exercises tailored for those focused on arthritis and joint health for active living.
- Total Gym: At a 45° incline with an elastic band around your knees, this exercise engages the gluteal medius, minimus, maximus, quadriceps, and hamstrings. It improves your ability in sitting, standing, climbing, and walking.
- Chair Squat: Adding a weighted backpack enhances resistance, targeting the gluteal maximus, quadriceps, and hamstrings. This aids in sit-to-stand motions, stair climbing, and walking.
- Knee Extension Machine: Operating within a pain-free range focuses on the quadriceps, improving your ability in sit-to-stand motions, stair climbing, and walking.
- Hamstring Curl: This also works within a pain-free range, targeting the hamstrings and enhancing your stair climbing and walking ability.
- Shoulder Press Machine: Using the front grip option avoids shoulder pain, working the deltoids and triceps for pushing and reaching overhead.
- Chest Press Machine: Limiting the descent range focuses on the deltoids, pectorals, and triceps, aiding in pushing activities.
- Bicep Curls: With resistance training gloves for stability, this engages the biceps, brachialis, and brachioradialis, aiding in carrying groceries and controlling a dog leash.
- Triceps Extension: Performed both standing and overhead; this targets all heads of the triceps, improving your pushing activities.
- Seated Rows: Maintaining scapular retraction and lumbar lordosis targets the latissimus dorsi, rhomboids, and middle trapezius, aiding in activities like controlling a dog leash and lifting groceries.
- Time-Based Gripping Putty: Progressive putty colours engage finger flexors, improving your ability to open jars and carry groceries.
- Time-Based Finger Adduction with Putty: This targets the finger adductors, aiding in tasks like opening jars and carrying groceries.
- Brisk Land-Based or Water Walking: On flat terrain or in waist-level water, this engages the gluteals, hamstrings, and quadriceps, improving walking endurance and lower extremity muscle performance.
- Chair Sit and Reach, Standing Lunch Calf Stretch: Avoiding ballistic movements while stretching focuses on the hamstring, gastrocnemius, and soleus, improving functional mobility for stair descent, walking, and deep squatting.
The FITT Framework
Building on our previous insights into arthritis and joint health for active living. Let’s explore the specifics of an exercise programme tailored for individuals with arthritis. The approach is rooted in the FITT framework, which stands for Frequency, Intensity, Time, and Type, and is adapted to consider the unique challenges and needs of those with arthritis. 1. Aerobic
- Frequency: Exercise 3-5 days per week.
- Intensity: Opt for moderate to vigorous intensity, gauged by 40%-59% VO2R (oxygen uptake reserve) or HRR (heart rate reserve).
- Time: Aim for 150 minutes per week of moderate-intensity or 75 minutes of vigorous intensity.
- Type: Choose low-joint stress activities like walking, cycling, swimming, or aquatic exercise.
2. Resistance
- Frequency: Exercise 2-3 days per week.
- Intensity: Start with 40-60% 1-RM (1 repetition maximum), especially if you’re new to resistance training.
- Time: Follow healthy adult values, typically 8-12 repetitions for 2-4 sets, including all major muscle groups.
- Type: Utilise machine or free weights. Body weight exercises might also be suitable for some.
3. Flexibility
- Frequency: Engage in daily stretching.
- Intensity: Move through ROM (range of motion), feeling tightness but avoiding pain.
- Time: Perform up to 10 repetitions for dynamic movements and hold static stretches for 10-30 seconds.
- Type: Combine dynamic and static stretching, focusing on all major joints.
This FITT framework allows for a customised exercise programme optimising arthritis and joint health for active living. 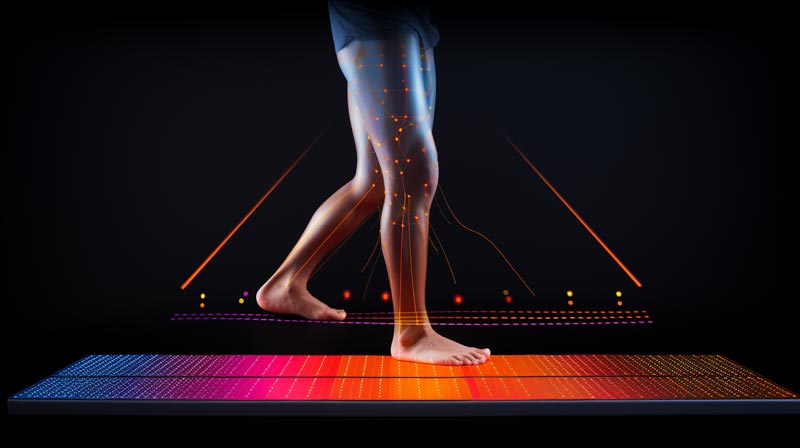
Safety Measures and Precautions for Exercising with Arthritis and Joint Health
Traversing the complexities of exercise while managing arthritis and joint health for active living requires a meticulously planned and adaptable approach. Understanding the dynamic nature of arthritis flare-ups is crucial. These aren’t merely inconvenient; they represent an acute immunological response that can seriously compromise joint function. During such episodes, recalibrating your exercise programmes is beneficial and medically advisable. Reducing the workout intensity or temporarily sidelining activities aggravating the symptoms could be the difference between a manageable condition and long-term joint damage. Joint instability, often an insidious byproduct of arthritis, is another critical concern. As the cartilage wears away, the surrounding tissues can’t maintain the joint’s natural alignment. The result is a slackening of the tissues that traditionally stabilise the joint, leading to a sensation known as “giving way.” This instability is not just uncomfortable, but it can be a precursor to more severe functional impairments. To counteract this, using orthotics or braces is a practical necessity that can improve quality of life. Moreover, exercise testing for individuals with arthritis isn’t business as usual. High-intensity workouts can exacerbate inflammation and are therefore contraindicated during flare-ups. The physiological stress of exercise can trigger an immunological response, worsening a bad situation. Therefore, pain levels during these tests should be closely monitored using validated scales like the Borg CR10 Scale. To ensure that the exercise programme doesn’t become a health risk. Individualised fitness assessments transcend the space of general advice. For arthritis sufferers, the stakes are higher. The risk of flares, grip weakness, and joint instability necessitates a customised approach that enhances physical performance and navigates the unique challenges posed by arthritis. Finally, a word on footwear: given the biomechanical complexities of arthritis, the right shoes are not a luxury but a necessity. Proper support and cushioning can correct minor alignment issues, minimising undue stress on already compromised joints. 
Living with Arthritis and Joint Health for Active Living: Fitness and Lifestyle Tips
Navigating the intricacies of arthritis is a complex task that extends far beyond the medical space; it demands a holistic approach grounded in scientific research, lifestyle adjustments, and proactive management strategies. As we’ve explored, arthritis and joint health for active living aren’t mutually exclusive. Comprehensive research-backed exercise programmes alleviate symptoms and contribute to an improved quality of life, both physically and mentally. Tackling arthritis successfully involves more than symptom alleviation; it requires a strategy to regain control of your life. The significance of an evidence-based approach must be considered. Exercise becomes a cornerstone in managing arthritis, with the power to transform lives. This comprehensive strategy empowers individuals to reclaim their active lifestyles and achieve a level of well-being that defies the limitations often associated with arthritis. Here are some points to take into consideration: 1. Exercise: A Cornerstone for Management Regular exercise is integral for managing Rheumatoid Arthritis (RA) and Osteoarthritis (OA). Aerobic and resistance training reduces disease activity, pain, and fatigue while enhancing physical function, muscle strength, and mental health. Aquatic exercise is another viable option, particularly for symptom relief. 2. Physical Activity: Beyond Just Exercise Physical activity is any bodily movement that expends energy, such as walking and gardening. Exercise is structured and repetitive, like swimming. Increasing physical activity can significantly improve disease-related and systemic outcomes, including reduced costs from fewer hospital admissions. 3. Medication and Supplements: The Exercise Connection Exercise may reduce the amount of medication taken for pain control. While supplements like glucosamine and chondroitin or fish oil may help, a healthy diet and maintaining an appropriate body weight are also crucial. 4. Individualised Exercise Programs Exercise programs should be tailored based on disease activity, joint involvement, and functional status. Start with low-intensity exercises and gradually increase duration and intensity, monitoring symptoms to ensure safety and efficacy. 5. Monitoring and Precautions It’s essential to monitor disease symptoms and adapt your exercise regime accordingly. Pain levels during or after workout sessions should be a guide to modify, eliminate, or replace exercises. New or worsening symptoms warrant immediate termination of activity and consultation with healthcare providers. 6. Barriers to Exercise Recognise barriers such as fatigue, lower baseline activity levels, and fear of detrimental effects. Overcoming these is necessary to effect a lifestyle change that incorporates exercise safely. The pathway to managing arthritis and maintaining joint health is complex and universal. Individualised exercise protocols, mindful lifestyle choices, and cutting-edge medical interventions converge to forge a lifestyle that accommodates the challenges and aspirations of living actively with arthritis. Our exploration into this subject has unveiled that exercise is not just a supplementary treatment; it’s a vital component that substantiates the overarching strategy for arthritis management. So, when discussing arthritis and joint health for active living, we’re talking about a lifestyle overhaul that spans the physical, emotional, and psychological dimensions. The guidelines and insights provided here serve as a comprehensive resource that not only guides you through the labyrinth of arthritis management but also instils a newfound sense of empowerment. With the right tools and knowledge, the limitations of arthritis can become mere hurdles, not impassable walls. The future of arthritis management is promising, teeming with innovative research and an ever-evolving understanding of how exercise and lifestyle factors intertwine with medical treatment. The endgame is clear: a life not merely survived but actively and vibrantly lived despite the challenges posed by arthritis.
Sources
- Al-Qubaeissy KY, Fatoye FA, Goodwin PC, Yohannes AM. The effectiveness of hydrotherapy in the management of rheumatoid arthritis: a systematic review. Musculoskeletal Care. 2013;11(1):3–18.
- Baillet A, Zeboulon N, Gossec L, et al. Efficacy of cardiorespiratory aerobic exercise in rheumatoid arthritis: meta-analysis of randomized controlled trials. Arthritis Care Res (Hoboken). 2010;62(7):984–92.
- Barrett, D.S., Cobb, A.G., Bentley, G. 1991. Joint proprioception in normal, osteoarthritic and replaced knees. J Bone Joint Surg Br. Jan;73(1):53-6.
- Bartels EM, Lund H, Hagen KB, Dagfinrud H, Christensen R, Danneskiold-Samsøe B. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD005523.
- Becker, R., Berth, A., Nehring, M., Awiszus, F. 2004. Neuromuscular quadriceps dysfunction prior to osteoarthritis of the knee. J Orthop Res. Jul;22(4):768-73.
- Belza BL. Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol. 1995;22(4):639–43. Bielefeld T, Neumann DA. The unstable metacarpophalangeal joint in rheumatoid arthritis: anatomy, pathomechanics, and physical rehabilitation considerations. J Orthop Sports Phys Ther. 2005;35(8):502–20.
- Borg GA. Scaling pain and related subjective somatic symptoms. In: Borg GA, editor. Borg’s Perceived Exertion and Pain Scales. Champaign (IL): Human Kinetics; 1998. p. 63–7.
- Bosch PR, Traustadottir T, Howard P, Matt KS. Functional and physiological effects of yoga in women with rheumatoid arthritis: a pilot study. Alt Ther Health Med. 2009;15:24-31.
- Brousseau L, Pelland L, Wells G, et al. Efficacy of aerobic exercises for osteoarthritis (part II): a meta-analysis. Phys Ther Rev. 2004;9:125-145.
- Durcan L, Wilson F, Cunnane G. The effect of exercise on sleep and fatigue in rheumatoid arthritis: a randomized controlled study. J Rheumatol. 2014;41(10):1966–73.
- Ferguson B. ACSM’s Guidelines for Exercise Testing and Prescription 9th Ed. 2014. J Can Chiropr Assoc. 2014 Sep;58(3):328. PMCID: PMC4139760.
- Fisher, N.M. 2002. Osteoarthritis, rheumatoid arthritis, and fibromyalgia. In: Myers, J.N., Herbert, W.G., Humphrey, R., editors. ACSM’s Resources for Clinical Exercise Physiology. Philadelphia (PA): Lippincott, Williams & Wilkins, p. 111–24.
- Fitzgerald, G.K., Piva, S.R., Irrgang, J.J. 2004. Reports of joint instability in knee osteoarthritis: its prevalence and relationship to physical function. Arthritis Rheum. Feb 15;50(1):40-8.
- Fitzgerald GK, Piva SR, Gill AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91:452-469.
- Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015 Dec;49(24):1554-7.
- Grover HS, Gaba N, Gupta A, Marya CM. Rheumatoid arthritis: a review and dental care considerations. Nepal Med Coll J. 2011;13(2):74–6.
- Häkkinen A. Effectiveness and safety of strength training in rheumatoid arthritis. Curr Opin Rheumatol. 2004 Mar;16(2):132-7. Hall A, Maher C, Latimer J, Ferreira M. The effectiveness of tai chi for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Arthritis Rheum. 2009;61:717-724.
- Hassan, B.S., Mockett, S., Doherty, M. 2001. Static postural sway, proprioception, and maximal voluntary quadriceps contraction in patients with knee osteoarthritis and normal control subjects. Ann Rheum Dis. Jun;60(6):612-8.
- Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012 Apr;64(4):465-74.
- Hurkmans, E., van der Giesen, F.J., Vliet Vlieland, T.P., et al. 2009. Dynamic exercise programs (aerobic capacity and/or muscle strength training) in patients with rheumatoid arthritis. Cochrane Database Syst Rev. Oct 7;(4):CD006853.
- Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018 Apr 23;4:CD010842.
- Hurwitz, D.E., Sumner, D.R., Andriacchi, T.P., Sugar, D.A. 1998. Dynamic knee loads during gait predict proximal tibial bone distribution. J Biomech. May;31(5):423-30.
- Iversen MD, Brawerman M, Iversen CN. Recommendations and the state of the evidence for physical activity interventions for adults with rheumatoid arthritis: 2007 to present. Int J Clin Rheumtol. 2012;7(5):489–503.
- Kaufman, K.R., Hughes, C., Morrey, B.F., Morrey, M., An, K.N. 2001. Gait characteristics of patients with knee osteoarthritis. J Biomech. Jul;34(7):907-15.
- Kelley GA, Kelley KS, Hootman JM, Jones DL. Effects of community-deliverable exercise on pain and physical function in adults with arthritis and other rheumatic diseases: a meta-analysis. Arthritis Care Res (Hoboken). 2011 Jan;63(1):79-93.
- Long, W.T., Dorr, L.D., Healy, B., Perry, J. 1993. Functional recovery of noncemented total hip arthroplasty. Clin Orthop Relat Res. Mar;(288):73-7.
- Mangione KK, McCully K, Gloviak A, Lefebvre I, Hofmann M, Craik R. The effects of high-intensity and low-intensity cycle ergometry in older adults with knee osteoarthritis. J Gerontol. 1999;54(A):M184-M190.
- McKean, K.A., Landry, S.C., Hubley-Kozey, C.L., et al. 2007. Gender differences exist in osteoarthritic gait. Clin Biomech (Bristol, Avon). Jun;22(5):400-9.
- O’Connor, B.L., Visco, D.M., Brandt, K.D., Myers, S.L., Kalasinski, L.A. 1992. Neurogenic acceleration of osteoarthrosis. The effects of previous neurectomy of the articular nerves on the development of osteoarthritis after transection of the anterior cruciate ligament in dogs. J Bone Joint Surg Am. Mar;74(3):367-76.
- Rindfleisch JA, Muller D. Diagnosis and management of rheumatoid arthritis. Am Fam Physician. 2005;72(6):1037–47.
- Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. 2010;376(9746):1094–108.
- Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2009 Nov 15;61(11):1545-53.
- Young IA, Cleland JA, Michener LA, Brown C. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil. 2010;89(10):831–9.
- Zamunér AR, Moreno MA, Camargo TM, et al. Assessment of Subjective Perceived Exertion at the anaerobic threshold with the Borg CR-10 Scale. J Sports Sci Med. 2011;10(1):130–6.


